RSM Blog: Sports Medicine and Massage Insights
Exploring Massage Therapy Career Options for the Serious Practitioner
The Modern Massage Landscape
Potential students often view the industry through too narrow a lens, assuming the profession is limited to spa environments. This misconception overlooks the rapid integration of manual therapy into mainstream healthcare. In my experience training practitioners at RSM Massage School in Thailand, I have observed that the most successful graduates are those who recognize early on that massage is a clinical tool, not just a luxury service.
The demand for skilled massage therapists has evolved significantly. Patients seeking pain relief for conditions like sciatica or frozen shoulder require a therapist who understands functional anatomy. Consequently, the work environment for modern practitioners has shifted from purely aesthetic settings to multidisciplinary clinics. This shift changes the trajectory of a career. When a therapist can demonstrate that their treatments resolve pathology rather than merely soothing symptoms, they unlock a tier of employment that offers greater stability.
To fully explore the potential of this field, one must look at the specific sectors where manual therapy is currently thriving. The options are vast, but they require distinct skill sets. A job in a palliative care unit demands a different approach than a position with a professional football team. Therefore, understanding the nuances of these environments is the first step in defining a viable career path.
Medical Massage and Therapy Career Pathways
One of the most rapidly growing sectors is the clinical environment. Here, massage therapy functions as a complementary component to orthopedic and rehabilitative care. In this setting, the therapist operates alongside physical therapists and osteopaths. This collaborative dynamic forces the therapist to adopt a medical vocabulary and a deeper understanding of pathology.
Medical massage specifically targets diagnosed conditions. Unlike general wellness sessions, these treatments follow a specific care plan devised to improve range of motion. Therapy in this context is result-oriented. For example, when treating a client with lateral epicondylitis (tennis elbow), the therapist must understand that the pain often originates from extensor muscle overload in the forearm, rather than just local inflammation.
Choosing this occupation path requires rigorous education. Massage schools that focus solely on Swedish massage rarely provide the depth of knowledge necessary for clinical work. Licensed massage therapists in medical settings must be proficient in orthopedic testing and nerve mobilization. The job outlook for clinical therapists is generally stronger than for generalists because patients and providers increasingly seek non-pharmacological pain management solutions.
Work Environments for Massage Therapists
At RSM International Academy, we specialize in sports medicine because it represents the pinnacle of functional manual therapy. Working in sports is demanding and requires the therapist to think critically about biomechanics. When an athlete presents with hamstring tightness, a standard therapist might simply rub the hamstring. In contrast, a sports-focused therapist analyzes the pelvic tilt and assesses lumbar mobility.
The environment in sports medicine is fast-paced. Massage therapists in this sector often travel with teams or work on the sidelines. The work involves pre-event preparation to prime the nervous system and post-event recovery to flush metabolic waste. This is a highly competitive career sector. Success here depends on the ability to deliver immediate, tangible results.
Athletes view their bodies as performance machines. If a therapist cannot explain the causal link between a treatment and improved performance, they will lose the client. Therapy careers in sports medicine often lead to high-profile opportunities, but they also carry higher expectations regarding liability and professional conduct.
Business Options vs. Job Stability
A critical decision for every practitioner is whether to seek employment or start a private business. Both career options have distinct advantages.
Employment offers stability. Working for a franchise or a medical clinic provides a steady stream of clients, handled administrative tasks, and predictable income. For new graduates, this is often the safest route to gain experience. However, the trade-off is often a lower per-hour salary compared to what self-employed therapists charge.
Conversely, private practice allows for total autonomy. A self-employed therapist sets their own rates and chooses their clients. This path appeals to those with an entrepreneurial spirit. However, it requires significant non-clinical work, such as marketing and legal compliance. In my observation, the highest earners are typically those who specialize in a niche area such as sports recovery, and run their own specialized services. They build a reputation for solving difficult cases, which allows them to command higher fees.
Wage Statistics and Job Outlook
When analyzing wage statistics and employment projections, it is vital to look beyond the averages. Government data often lumps all practitioners together, from entry-level spa workers to elite sports therapists. This aggregation can skew the perceived potential of the profession.
General occupational outlook data suggests that the field is growing faster than average. This growth is driven by an increased public awareness of the benefits of therapy. However, the salary range is wide. Entry-level positions in chain spas often pay near minimum wage. In contrast, occupational specialists in medical or sports settings can earn significantly more.
The job outlook is particularly robust for those with advanced certifications. As healthcare providers increasingly refer patients for manual therapy, insurance reimbursement is becoming more common. Projected growth is highest in metropolitan areas where integrative health centers are becoming the norm.
Determining Your Career Path and Finding Jobs
The foundation of a successful massage career is education. The curriculum a student chooses dictates their future options. Many generic programs focus on meeting minimum licensure requirements. While this allows a student to legally work, it often leaves them unprepared for complex clinical cases.
At RSM, we emphasize that education does not stop at graduation. Therapists who rely on outdated modalities eventually stagnate. Those who continue to explore new techniques and scientific findings maintain a competitive edge. Advanced training also protects the therapist’s own body. Poor body mechanics lead to injury and burnout. High-quality education teaches therapists how to use leverage to deliver deep pressure without compromising their own joints.
Integrating into the broader healthcare system presents specific challenges for finding jobs. Medical massage practitioners must navigate the complexities of patient documentation and inter-professional communication. A doctor referring a patient expects a SOAP note using standard medical terminology. If a therapist describes a session using vague language, they lose credibility. However, if they describe the treatment in terms of reducing hypertonicity to alleviate pelvic obliquity, they establish themselves as a peer.
Services provided in a healthcare setting are scrutinized for efficacy. Patients are often there because they are in pain, not because they want to relax. This changes the dynamic of the client-therapist relationship. Empathy remains crucial, but clinical competence takes precedence.
Entering the field of manual therapy is a commitment to lifelong learning. The options available today are far more diverse than they were twenty years ago. From the sidelines of professional sports to the quiet focus of a rehabilitation clinic, the role of the therapist has expanded. By choosing the right education, understanding the market dynamics, and treating the profession with the seriousness it deserves, new practitioners can build a rewarding and sustainable career. The key is to never stop analyzing and never underestimate the profound impact of skilled touch on the human body.
Analyzing the Physiological Benefits of Deep Tissue Massage
While teaching RSM's Deep Tissue Massage Course, I often notice that students over-rely on increasing force to address chronic pain. They assume that if the client feels pain, the therapy is working. In reality, effective deep tissue massage is not about how hard you push; it is about how precisely you engage the anatomical layers.
When we strip away the spa-like generalizations, the benefits of deep tissue massage reveal themselves as a sophisticated interaction between mechanical manipulation and neurological response. My experience in sports medicine has taught me that pain in a specific muscle belly is often just the symptom of a silent, rigid adhesion in the surrounding fascia. Consequently, to truly resolve the issue, a therapist must visualize the three-dimensional architecture of the body.
Analyzing the Clinical Benefits of Deep Tissue Massage
The primary goal of deep tissue massage is to restore the structural integrity of the musculoskeletal system. Unlike relaxation-based modalities, this form of massage focuses on realigning the deeper layers of muscle and connective tissue. When a massage therapist applies sustained pressure to these layers, they are mechanically shearing the cross-links that form between muscle fibers.
In a healthy state, muscles and fascia glide effortlessly over one another. However, chronic stress and repetitive strain cause these layers to adhere, creating a rigid environment where nutrients cannot enter. This ischemia (lack of blood flow) sensitizes nociceptors; the nerves that detect pain. Deep tissue massage intervenes by physically separating these adhered layers. This mechanical separation restores the glide potential of the tissue, allowing the muscle to contract without restriction.
How Deep Tissue Massage Remodels Fibrotic Tissue
In our curriculum, we emphasize that tissue is a dynamic variable. When the body sustains stress or injury, it lays down collagen fibers in a haphazard pattern to patch the area, forming fibrosis or scar tissue. While protective, an excess of fibrotic tissue restricts mobility.
Deep tissue massage acts as a remodeling force. The slow, concentrated strokes introduce a controlled micro-trauma to these fibrotic areas. This stimulus signals the body to break down disorganized collagen and replace it with pliable, linear fibers. Specifically, we often see this in the lateral thigh fascia. By engaging the deep interface between the quadriceps and hamstrings, the massage therapist can free the lateral chain, leading to reduced tension on the knee joint.
The Science of Deep Pressure and Massage Mechanics
There is a precise science to how deep pressure influences the nervous system. A common misconception is that deep tissue massage must be excruciating. This is false. If the pressure is too aggressive, the client’s body enters a sympathetic “fight or flight” state, causing muscles to guard.
Instead, effective deep tissue work operates on the “edge” of resistance. The therapist sinks into the tissue until they meet the barrier. At this depth, the pressure stimulates mechanoreceptors which lower sympathetic tone. This triggers a parasympathetic response, signaling the brain to drop tension levels. Consequently, the massage becomes a dialogue between the practitioner and the client’s nervous system. The release is neurophysiological, not just mechanical.
Differentiating Deep Tissue Protocols
It is important to clarify the distinction between deep tissue massage and Swedish massage. Swedish massage primarily aims to promote relaxation using long, gliding strokes. In contrast, deep tissue massage is corrective.
We utilize specific techniques to address dysfunction:
- Stripping: Deep gliding along muscle fibers.
- Friction: Pressure across the grain to break adhesions.
- Myofascial Release: Sustained pressure to release fascia.
Because the focus is on the deep structure, the massage therapist uses stronger levers, forearms and elbows, to apply consistent force without fatigue. This allows for the manipulation of dense tissue layers that standard massage cannot reach.
Deep Tissue Massage for Chronic Pain and Tissue Recovery
Chronic pain is often the cumulative debt of unresolved dysfunction. Patients with conditions like plantar fasciitis or lower back pain often find standard treatments insufficient because the source lies in the deeper strata of the soft tissue. Deep tissue massage addresses this via the “Pain Gate Theory.” By stimulating sensory fibers with non-noxious pressure, we block pain signals, providing a window of pain relief.
Furthermore, this therapy is essential for muscle recovery following exertion. Athletes accumulate metabolic byproducts like lactate. Tight muscles trap these fluids, leading to soreness. Deep tissue massage acts as a mechanical pump, flushing out stagnant fluid from the interstitial spaces. This exchange accelerates recovery and helps reduce pain associated with stiffness.
Overcoming Ischemia to Improve Circulation
Circulation is the lifeblood of tissue health. Ischemia contributes to degeneration. Deep tissue massage reverses this state. By manipulating deep muscle bellies, we mechanically dilate blood vessels, leading to hyperemia.
This ability to improve circulation extends beyond the local area. The systemic increase in blood flow lowers vascular resistance. For clients with tension headaches, relieving tension in the suboccipital muscles through deep tissue work restores cranial circulation, offering immediate health benefits.
Integrating Massage Therapy into Rehabilitation
At RSM International Academy, we teach that massage therapy is a potent tool within rehabilitation. When a client is recovering from injury, deep tissue massage prepares the tissue for strengthening. You cannot strengthen a muscle inhibited by trigger points.
The therapist plays a crucial role in breaking the pain-spasm-pain cycle. By carefully relaxing muscle spasms, we reduce inflammation markers locally. We also utilize lymphatic drainage techniques within deep tissue protocols to clear inflammatory mediators. This sets the stage for effective physical therapy.
Frequency of Sessions and Safety
For long-term improvement, consistency is key. Deep tissue massage is cumulative. One session may release superficial tension, but deep holding patterns require repeated inputs. We recommend a series of massage sessions to break the pattern of dysfunction.
However, safety is paramount. We do not apply deep pressure over acute inflammation or open wounds. A skilled therapist knows when to back off. The goal is to aid recovery, not induce injury.
The Corrective Power of Manual Therapy
The effectiveness of this modality lies in its specificity. It is a surgical approach to soft tissue dysfunction. Through improved circulation, the breakdown of scar tissue, and neurological resetting, deep tissue massage offers a pathway out of chronic pain.
For those training to become therapists, remember: your understanding of the tissue is your true power. When you combine anatomical knowledge with the skilled application of deep tissue massage, you do not just relax your client, you rebuild them.
Key Takeaways
- Precision: Effective deep tissue massage targets specific layers.
- Hydration: Water supports the metabolic flush after massage sessions.
- Consistency: Chronic pain requires consistent massage work to resolve.
- Health: Deep tissue work supports overall health and performance.
At RSM International Academy, we believe that deep tissue massage, when performed with clinical expertise, is one of the most powerful methods available for maintaining physical health.
Balancing Theory and Practical Learning in Advanced Massage Therapy
Anatomy is often understood in the static sense found in textbooks, which overlooks its critical role in dynamic movement and injury rehabilitation. Students who have memorized anatomical terms usually lack the tactile understanding of the true mechanical origins of pathology. At RSM Massage School here in Chiang Mai, we emphasize that physiological concepts are not just abstract definitions; they are dynamic variables that change based on load, posture, and tissue quality.
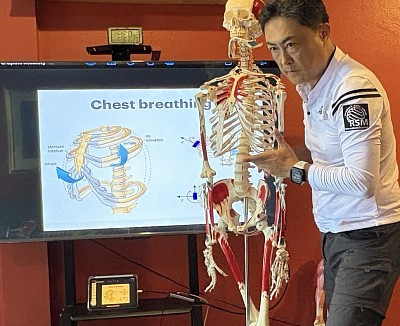
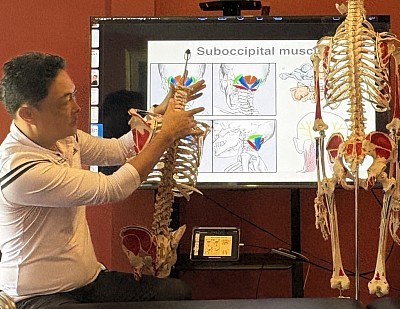
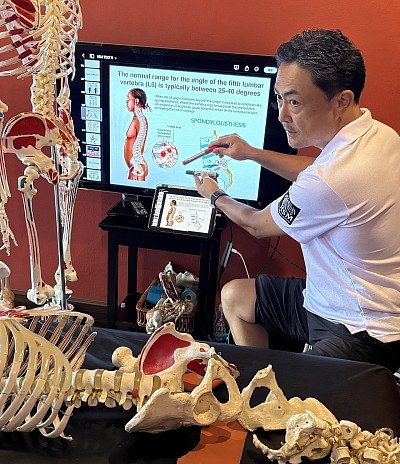
To truly master sports medicine-based massage, a therapist must move beyond simple memorization and start visualizing the three-dimensional relationship between structure and function. We do not view the classroom and the treatment table as separate entities. Instead, we treat them as a feedback loop where intellectual understanding drives manual precision, and tactile feedback refines intellectual models.
The Disconnect Between Theoretical Knowledge and Real Application
In traditional massage schooling, there is often a rigid separation between lecture and clinic. Students absorb theoretical knowledge regarding muscle origins and insertions to pass a written exam. Later, they enter a practical module to learn a set routine. This segmentation creates a dangerous gap. A student may know that the sciatic nerve is near the piriformis, but when a client presents with deep gluteal pain, they often fail to differentiate between pathologies because they haven’t learned to translate that knowledge into their hands.
This disconnect leads to generic treatments. If a therapist cannot translate their understanding of pathophysiology into their touch, they default to “rubbing where it hurts.” In sports medicine, this is insufficient. Pain is often a symptom, not the root cause. Without the ability to bridge theoretical concepts with hands-on assessment, the therapist addresses the symptom while the underlying dysfunction remains.
Redefining Education in the Classroom
We approach education differently, believing that teachers must act as clinical guides. In our classroom, a lecture on the lumbar spine does not end with a slide presentation. Immediately following the explanation of the facet joints, we move to the tables to palpate them through the layers of fascia. This method forces the brain to encode information differently, transforming abstract data into sensory data.
This approach requires a specific kind of teacher education. Our instructors are not just delivering content; they are demonstrating how to think like a clinician. By vocalizing their thought process during a demonstration, they model the internal dialogue of problem-solving. This teaches the student to construct their own clinical reasoning pathways, a skill far more valuable than memorization.
Why Practice Must Anchor Abstract Concepts
Intellectual concepts are easily forgotten without a physical anchor. Practice serves as this anchor. When a student reads about the “end-feel” of a joint, it remains a vague idea. It only becomes a clinical tool when they feel the hard stop of elbow extension compared to the firm, springy stop of a healthy knee joint.
We utilize specific practical exercises designed to heighten proprioception and precision. Teaching the depth of pressure required to access the psoas major cannot be learned from a book; it requires repeated, supervised execution. This physical discipline supports the intellectual work. Practical proficiency also involves the therapist’s own body mechanics. A therapist who understands leverage theory but cannot apply it through their own body will be inefficient and prone to injury.
Integrating Research Findings into Daily Treatment
The field of sports medicine is not static, as new research findings constantly challenge old dogmas. For years, static stretching before performance was common practice. However, current research shows that it can temporarily reduce power output. We integrate these updates directly into our practical training, teaching students to evaluate sources critically. This creates a culture of experiential learning where students can test hypotheses in real-time.
The Role of Models in Visualizing Pathology
While hands-on experience is paramount, anatomical models are invaluable for visualizing structures. This is particularly important for deep structures that are inaccessible to direct touch. Theoretical visualization helps prevent injury. If a therapist understands the intricate path of the brachial plexus, they will approach the lateral neck with appropriate caution. We use models to demonstrate these critical areas, ensuring that when a student touches a human body, they are seeing through the layers with their mind’s eye.
Experiential Learning and the Clinical Reasoning Loop
The ultimate goal of combining theory with hands-on work is to develop a therapist capable of independent clinical reasoning. This is a cyclical process we call the Clinical Reasoning Loop.
- Assessment (Theory/Practice): The therapist uses theoretical knowledge of biomechanics to observe movement and practical palpation skills to assess tissue.
- Hypothesis (Theory): Based on the data, the therapist forms a working hypothesis about the root cause of the dysfunction.
- Treatment (Practice): The therapist selects and applies a technique designed to address the hypothesis.
- Re-Assessment (Learning): Immediately after the intervention, the therapist re-tests.
- Adjustment (Synthesis): If the intervention was not successful, the hypothesis was incorrect or the technique was insufficient. The therapist adjusts and begins the loop again.
This loop turns every session into a micro-experiment and is central to our learning philosophy. It elevates the therapist from a technician following a script to a clinician who solves problems. We also provide students with the resources to continue this growth long after graduation, teaching them to build their own case logs and recognize when to refer a client to another specialist.
Bridging the Gap for Elite Therapy
The separation of head and hand is the enemy of mastery in manual therapy. A therapist with brilliant hands but no theoretical grounding cannot adapt to complex injuries. Conversely, an academic with encyclopedic knowledge but poor hands cannot effect change in the tissue.
At RSM International Academy, we recognize that the human body is the ultimate teacher. Our curriculum is designed to give you the language to understand what the body is telling you (theory) and the skills to respond effectively (practice). By rigorously integrating these two domains, we produce therapists who are ready for the demands of elite sports medicine. We train them not just to massage muscles, but to analyze movement, identify dysfunction, and restore performance. This is the only path to achieving true excellence in our field.
Deep Anatomy Knowledge for Orthopedic Massage
It's important for us to distinguish between relaxation therapy and clinical remediation. In our sports medicine curriculum, we teach that effective treatment relies on visualizing the three-dimensional machinery beneath the skin. To resolve chronic pain rather than merely masking it, a therapist requires specific anatomy knowledge, and a practical understanding that goes far beyond basic textbook definitions.
Elevating Massage Techniques Through Anatomy
The transition from relaxation-based work to clinical therapy demands a shift in cognitive approach. Standard massage often employs broad, non-specific strokes aimed at general circulation. In contrast, the techniques learned during RSM's Orthopedic Massage Course require pinpoint accuracy. When we treat a client, we are navigating a complex map of the musculoskeletal system.
If a practitioner lacks a deep knowledge of how layers interact, their massage becomes a guessing game. They might press hard on a structure that requires gentle release or stretch a tissue that is already over-lengthened. Consequently, the ability to palpate effectively is directly dependent on the therapist’s mental blueprint of anatomy. This understanding allows us to differentiate between a healthy tendon and a fibrotic adhesion, ensuring that every stroke has a clear therapeutic intent.
Precision in the Shoulder and Upper Limb
To illustrate the importance of this knowledge, consider the shoulder and arm. This region is dense with neurovascular structures, making precise muscle anatomy crucial for both safety and efficacy.
A superficial approach might focus solely on the deltoid muscle when a client reports shoulder pain. However, the deltoid often compensates for deeper dysfunction in the rotator cuff or scapular stabilizers. A therapist must understand these mechanical relationships to restore function.
Moving distally to the elbow, the need for specificity increases. Many massage therapists struggle to differentiate between the structures originating at the medial epicondyle versus the lateral epicondyle.
- Lateral Pain: Often involves the forearm extensor group. Specifically, the extensor carpi radialis brevis is a frequent driver of pathology. However, the brachioradialis muscle also exerts force here. A skilled therapist must palpate the septum between these muscles to release them individually.
- Medial Pain: Conversely, pain at the inner elbow involves the common flexor tendon, where the flexor carpi radialis and ulnaris converge.
- Safety: The cubital fossa (anterior elbow) contains the median nerve and brachial artery. Without precise knowledge of anatomy, a therapist risks compressing these sensitive structures while attempting to treat the distal biceps.
Sustainable Relief and Therapeutic Outcomes
Ultimately, the goal of orthopedic massage is sustainable relief. Clients seek our help because they are in pain or restricted in their movement, and generic approaches have failed them. By grounding our therapy in origins insertions and biomechanics, we offer a logical solution.
When we explain to a client that their elbow pain stems from specific forearm extensor tension, or that their shoulder restriction is linked to scapular mechanics, the treatment becomes educational. This therapeutic partnership encourages the client to trust the process. At RSM, we believe that you cannot fix a machine if you do not understand the blueprint. Therefore, mastering the detailed anatomy of the body is the most critical step in becoming an elite massage practitioner.
The Approach at Our International Massage School in Thailand
A Clinical Perspective on Massage Education
When I established RSM International Academy in Chiang Mai, my objective was to bridge the significant divide between generalized relaxation and clinical therapeutic treatment. In the world of manual therapy, there is an abundance of training focused on sequence memorization. However, memorizing a sequence does not equate to understanding the body. True therapy requires a diagnostic mind. Consequently, we built a curriculum rooted in Dynamic Postural Assessment and science backed sports medicine.
At our massage school here in Thailand, we teach students that the source of pain is rarely where the client points to. It is usually the result of a kinetic chain dysfunction. Consider a client with chronic lower back pain. A standard therapist might apply deep pressure to the lumbar erectors. This often fails because the pain is merely a symptom. In many cases, the root cause lies in a restricted ankle dorsiflexion or a tight iliopsoas. When the psoas shortens, it inhibits the gluteus maximus. As a result, the lumbar extensors overwork to maintain posture, leading to fatigue and pain.
Our training emphasizes this causal logic. We do not simply teach how to rub muscles; we teach how to assess structural integrity. By understanding functional anatomy, a therapist transforms from a service provider into a clinician.
A Scientific Foundation for Clinical Massage
Our methodology is intentionally distinct from the conventional spa models prevalent in Thailand. While relaxation has its place, our mission is to provide an evidence-based education focused on pain relief. We founded this academy on the principles of sports medicine and clinical palpation.
Instead of teaching a generalized routine, we teach a process of assessment and treatment. This style of education requires deep biomechanical knowledge. Students learn to perform orthopedic tests to form a clear clinical picture before beginning hands-on work. This elevates the practice of massage from a generic service to a targeted intervention. The goal is to produce lasting changes in function.
The Difference in Our School Curriculum
The curriculum at RSM is designed for those who seek to elevate their practice. We limit class sizes to ensure every student receives direct feedback. Large classes often result in students mimicking movements without understanding tissue texture. In our courses, tactile sensitivity is prioritized.
We structure our learning environment to focus on:
- Functional Anatomy & Cadaver Study: We go further than standard charts by offering the world’s first massage course with hands-on cadaver palpation training, in collaboration with the Faculty of Medicine at Chiang Mai University.
- Trigger Point Therapy: We teach students to locate taut bands and identify referral patterns. For instance, a headache is often caused by active trigger points in the Sternocleidomastoid (SCM) rather than pathology in the head.
- Deep Tissue Massage & Myofascial Release: True deep tissue massage is about sinking into the fascia, not applying brute force. Our Dynamic Myofascial Release course integrates this with joint mobilization.
This training program is rigorous. It demands that students study outside of practical hours. Because the human body is complex, the learning curve is steep. However, the reward is the ability to resolve chronic pain conditions other therapists have failed to treat.
Advanced Training Beyond a Standard Massage School in Thailand
Standard vocational schools often adhere to curriculums that prioritize safety over efficacy. While our courses are approved by relevant authorities, we view the standard curriculum as a starting point. We push beyond the basics into advanced manual therapies.
Key differentiators include:
- Osteopathic Integration: We incorporate joint mobilization techniques to restore sliding surfaces within the articular capsule.
- Kinetic Chain Assessment: We teach Dynamic Posture Assessment to identify how misaligned movement patterns lead to pain.
- Sports Medicine Protocols: We customize treatments for injury prevention. A runner with shin splints needs a different protocol than a weightlifter with shoulder impingement.
We also focus on longevity. Many careers end due to injury. We teach body mechanics that utilize leverage rather than muscular effort. By stacking the joints and generating force from the core, our students learn to deliver deep pressure for hours without fatigue. This sustainability is crucial for a long-term career in massage education and practice.
To illustrate our depth, consider “Sciatica.” Many clients actually suffer from Pseudo-Sciatica caused by the Gluteus Minimus. Trigger points here refer pain down the leg, mimicking nerve compression. If a therapist treats the spine for a disc issue that doesn’t exist, the client gets no relief. By palpating the Gluteus Minimus, our students reproduce and resolve the pain. This diagnostic accuracy is what defines an international massage specialist.
RSM International Academy is not for those seeking a holiday course. It is for serious practitioners. We provide a massage school experience that challenges the intellect. By focusing on a sports medicine-based approach, we equip graduates to make a profound impact on their clients’ health.
Ergonomics for Sports Massage Professionals: A Sports Medicine Approach
Many massage therapists view ergonomics merely as a set of workplace safety guidelines, overlooking its critical role in the efficiency of force transmission. In my experience training students at RSM International Academy, I often have to explain that the pain a practitioner feels in their lower back or thumb is not just an occupational hazard; it is a sign of a broken kinetic chain. When a therapist generates force solely from their upper body rather than transmitting it from the ground up, they are not only risking injury but also delivering a suboptimal treatment.
To truly master deep tissue and sports massage, a practitioner must move beyond simple memorization of client anatomy and start visualizing the three-dimensional relationship between their own body mechanics and the client’s tissue response. In RSM's Sports Massage Course, we emphasize that the therapist is, in essence, an athlete. Your event is the massage session, and your performance depends entirely on how well you manage your own biomechanical load.
The Biomechanics of the Therapist: Why Posture Failures Occur
In our curriculum, we emphasize that posture is not a static position but a dynamic state of readiness. When a massage therapist stands at the table, they create a closed kinetic chain. The force applied to the client does not originate in the hands; it begins at the feet, travels through the legs, crosses the pelvis, stabilizes through the spine, and finally exits through the contact point.
If any link in this chain is weak or misaligned, the body compensates. Specifically, if a practitioner lacks core stability, the lumbar spine takes the load. This leads to a common error where the therapist tries to “push” into the tissue using triceps strength. This muscular effort creates tension in the therapist’s own trapezius and levator scapulae. Consequently, the client feels a “sharp” pressure rather than a deep, sinking engagement.
Effective mechanics rely on the principle of stacking. By aligning the shoulder, elbow, and wrist directly over the contact point, the skeleton bears the load rather than the muscles. This skeletal stacking allows the therapist to lean their body weight into the stroke, utilizing gravity as a primary energy source. This approach reduces metabolic expenditure and minimizes the risk of burnout.
Analyzing Common Injuries in Massage Therapy
I frequently encounter cases of career-ending injuries labeled as “overuse.” In fact, the problem often begins far from the site of pain. The chain typically starts with a minor mechanical fault, such as working with a high center of gravity. This fault increases torque on the lower back, promotes shoulder elevation, and lays the foundation for chronic inflammation.
The Wrist and Kinetic Chain Failure
One of the most frequent corrections I make is when students attempt to address deep restrictions by solely focusing on thumb pressure. The thumb’s saddle joint is inherently unstable under direct compression. When a massage therapist relies on their thumbs for deep tissue work, they subject a small surface area to massive force.
This mechanical stress often results in De Quervain’s tenosynovitis. In contrast, using the olecranon (elbow) changes the physics of the interaction. By broadening the contact tool, we distribute the force over a larger surface area. Common injuries like carpal tunnel syndrome often stem from working with the wrist in extension. Once the wrist deviates beyond 15 degrees of extension while under load, pressure within the carpal tunnel rises, compressing the median nerve.
Lower Back Pain and the Hip Hinge
The back is perhaps the most vulnerable area for massage therapists. A significant percentage of issues in our field are lumbar strains caused by the “topple” effect. This occurs when a therapist bends at the waist to reach a client on the far side of the table, creating a long lever arm that places immense shear force on the L4 and L5 vertebrae.
To neutralize this ergonomic risk, practitioners must master the hip hinge and the lunge stance. By keeping the spine neutral and bending at the hips and knees, the therapist lowers their center of gravity. This shifts the load from the small erector spinae muscles to the powerful gluteals. At RSM, we integrate this movement pattern into our practice, ensuring that every stroke is powered by the legs.
Optimizing the Massage Table and Equipment Setup
The massage table is the primary workbench of our profession, yet it is often the source of dysfunction. Many therapists set their table height based on visual symmetry rather than biomechanical leverage. A table set too high forces the therapist to elevate their shoulders to generate downward pressure, leading to tension headaches.
Conversely, a table that is too low forces the therapist to flex the lumbar spine to maintain contact. This compromises the core and places the lower back in a vulnerable position. While the standard “fingertip rule” is a good starting point, for deep tissue or sports massage, I often recommend setting the equipment slightly lower. This allows the practitioner to utilize more of their body weight for downward compression without bending the elbows.
Equipment safety also extends to the flooring. Working on a hard surface without shock absorption prevents the feet from making micro-adjustments. This rigidity travels up the chain, locking the knees and hips. Investing in high-quality supportive footwear allows for dynamic footwork, which is essential for transferring weight effectively.
Workplace Posture and Dynamic Movement
Static posture is the enemy of the massage therapist. Standing in one position for an hour-long treatment causes blood pooling in the lower extremities and fatigue in the postural muscles. In our training, we treat the massage session as a dance. The therapist must constantly shift their weight from the back foot to the front foot.
This concept of “dynamic work ergonomics“ implies that the therapist is never truly still. Even during a static compression technique, the therapist should be micro-adjusting their center of gravity. For therapists who perform seated work, a saddle stool can maintain the natural lumbar curve better than a flat chair. The saddle shape forces the hips into an open angle, reducing the tendency to slouch.
Identifying Ergonomic Hazards and Corrective Practice
Ergonomic hazards are not limited to the physical mechanics of the session. The “invisible” load of the profession, scheduling and mental focus, plays a massive role in injury rates. Massage tasks that require repetitive high-force output deplete glycogen stores and fatigue the nervous system. When the nervous system is fatigued, proprioception degrades, leading to sloppy mechanics late in the day.
We advise our students to structure their day with “active recovery” blocks to prevent repetitive strain on specific muscle groups. Ultimately, the longevity of a massage therapist depends on their commitment to self-care. At RSM International Academy, we do not view self-care as a luxury; it is a professional responsibility. If your neck is stiff or your health is compromised, your ability to palpate tissue restrictions is diminished.
We recommend a daily practice of corrective exercises designed to reverse the postures of the workplace:
- Thoracic Extension: Reversing the kyphotic curve developed from looking down at clients.
- Forearm Stretching: Releasing tension in the flexor compartment.
- Gluteal Activation: Ensuring the glutes remain the primary drivers of force.
By treating our own bodies with the same level of clinical rigor that we apply to our clients, we ensure that we can continue to practice this demanding craft for decades. By respecting the laws of biomechanics and recognizing the risk factors inherent in our trade, we elevate the standard of care for everyone.
Shiatsu Acupressure Points Explained by a Sport Medicine Teacher
Many students initially view shiatsu as purely energetic. They memorize locations without understanding the underlying tissues. However, my experience in sports medicine suggests that this approach limits efficacy. When we analyze the classical locations of these targets, we almost invariably find that they correspond to motor points, neurovascular bundles, or areas of dense fascial convergence.
The “magic” of acupressure is not in the chart, but in the application. It lies in understanding how pressure applied to specific coordinates influences the nervous system and alters muscle tone. RSM's Shiatsu Massage Course bridges the gap between traditional wisdom and modern anatomical science.
The Science Behind Acupressure Massage
While traditional texts explain acupressure through the movement of Qi (life energy), modern sports medicine offers a physiological parallel crucial for the evidence-based therapist. When we stimulate specific areas, we engage in mechanotransduction. This is the process by which cells convert mechanical stimulus into biochemical activity.
The concept of meridians aligns remarkably well with what Thomas Myers describes as “Anatomy Trains” or myofascial kinetic chains. For example, the Urinary Bladder meridian runs parallel to the Superficial Back Line. A restriction in the plantar fascia often transmits tension up to the sub-occipital region.
Treating these pathways is not just about balancing abstract energy; it is about releasing fascial adhesions that compromise movement efficiency. Consequently, effective acupressure massage does more than relax a client. It restores the glide between tissue layers. By targeting high-resistance areas along these chains, we reduce mechanical drag on the musculoskeletal system, leading to improved range of motion and a reduction in compensatory patterns.
Defining Pressure Points and Tsubos
In the Japanese tradition, the specific locations we treat are called “Tsubos.” A Tsubo is often described as a vessel where tension accumulates. Clinically, these spots are rarely random. A skilled palpation assessment usually reveals that a Tsubo corresponds to a trigger point or a myofascial adherence.
Pressure points are areas of high electrical conductivity and lower skin resistance compared to the surrounding tissue. When a therapist applies perpendicular force to these areas, several physiological responses occur:
- Ischemic Compression: Temporary restriction of blood flow causes a reactive hyperemia upon release, flushing out metabolic waste products like lactic acid.
- Neurological Gating: Strong, non-painful stimulation of large sensory fibers blocks the transmission of pain signals from smaller fibers at the spinal cord level.
- Autonomic Switching: Sustained, deep pressure stimulates the vagus nerve, shifting the body from a sympathetic state to a parasympathetic state.
Understanding this biology changes the intent of the treatment. We are communicating with the central nervous system to downregulate pain signals and reset muscle tone.
Mastering Shiatsu Technique
The defining characteristic of shiatsu is the quality of touch. Unlike other forms of massage that utilize friction, this modality relies on static, perpendicular penetration. The Japanese term literally translates to “finger pressure,” but the technique requires the use of the whole body’s weight, not just the strength of the thumb.
Many therapists fail because they use muscle strength to push, resulting in a “poking” sensation. Conversely, correct shiatsu technique involves stacking the joints—shoulder over elbow, elbow over wrist—and leaning body weight into the recipient.
This static pressure allows the tissue to melt. When we apply a rubbing motion, the muscle spindle fibers often react by contracting. By keeping the hand pressure stable, we bypass this stretch reflex. The nervous system accepts the intrusion, allowing access to deeper layers without eliciting a defensive guarding response.
Mapping Specific Acupoints to Anatomy
At RSM, we train students to locate points via palpation rather than visual measurement alone. However, knowing the anatomical correlation is essential. Here, we analyze key acupressure points used in sports recovery.
GB21 (Jian Jing)
Located at the highest point of the shoulder.
- Anatomical Correlate: Direct access to the upper trapezius belly and supraspinatus.
- Clinical Application: A primary target for tension headaches. In overhead athletes, the upper trapezius often becomes dominant. Releasing GB21 helps restore scapular mechanics.
- Caution: This area contains the lung apex. While deep needle insertion in acupuncture carries risks, manual pressure is generally safe.
LI4 (He Gu)
Located on the dorsum of the hand, between the first and second metacarpals.
- Anatomical Correlate: The first dorsal interosseous muscle and adductor pollicis.
- Clinical Application: Famous for general pain relief. As the distal terminus of the arm lines, releasing high-tone intrinsic hand muscles creates a reflex relaxation effect up the entire arm chain.
ST36 (Zu San Li)
Located four finger-widths below the patella, lateral to the tibial crest.
- Anatomical Correlate: The tibialis anterior muscle.
- Clinical Application: Critical for runners, as the tibialis anterior governs ankle dorsiflexion. Tightness here leads to shin splints. Treating ST36 directly addresses hypertonicity in the anterior compartment.
BL23 (Kidney Shu)
Located in the lumbar region at the L2 level.
- Anatomical Correlate: Accesses the erector spinae and Quadratus Lumborum (QL).
- Clinical Application: The QL is often the culprit in non-specific low back pain. Deep, sustained pressure here releases deep stabilizing muscles that standard surface massage often misses.
Applying Pressure for Clinical Effect
The effectiveness of acupressure depends entirely on the dosage of force. We teach a concept called “sinking.” The therapist makes contact with the skin and waits. As the superficial fascia relaxes, the therapist sinks to the muscle layer, and finally to the depth of the pressure point.
Western medicine often dismisses “Qi” or energy flow. However, if we interpret “blockage of Qi” as “impediment to blood flow,” the concepts align. When a muscle is hypertonic, it compresses vasculature, creating a local hypoxic environment. By releasing these restrictions through points massage, we restore oxygenated blood flow, allowing cellular repair to function optimally.
Furthermore, the modern athlete is often stuck in a state of sympathetic dominance—high stress and constant alertness. Recovery cannot occur in this state. Acupressure is a potent tool for flipping this switch. The rhythmic pressure stimulates proprioceptors, slowing the heart rate and restoring autonomic balance. Without this systemic shift, local tissue work provides only temporary relief.
Integrating Acupressure Techniques
At RSM International Academy, we do not view shiatsu acupressure as a standalone cure-all. Instead, it is a vital component of a comprehensive rehabilitation strategy. A therapist might use these techniques to release a hypertonic antagonistic muscle before asking the client to perform a strengthening exercise.
For instance, if a client has limited knee extension due to tight hamstrings, stretching alone may trigger the stretch reflex. Applying pressure to the hamstring acupoints first downregulates the tone. This creates a neurological window where the muscle is more compliant, making subsequent mobility work significantly more effective.
The study of shiatsu acupressure provides a map to the body’s most influential neuromuscular junctions. By understanding the anatomy under the points, the physiology of pressure, and the mechanics of the kinetic chain, a therapist transforms a simple treatment into a targeted medical intervention. Whether addressing chronic pain or acute tightness, we locate the restriction, apply precise force, and wait for the nervous system to respond. This fusion of ancient technique and modern science defines our standard of care.
The Clinical Benefits of Remedial Massage Training
Many therapists view their initial education as a static foundation, overlooking the critical role that advanced diagnostic skills play in long-term treatment success. One of the most frequent corrections I make during practical training in RSM's Remedial Massage Course is when students attempt to address pain by solely focusing on the site of symptoms. In my experience, the pain a client feels in their lower back is often a compensatory price they are paying for stiffness in the hip or restriction in the ankle. This distinction between treating symptoms and identifying root causes is what defines the transition from a standard therapist to a clinical practitioner.
To truly master this field, a therapist must move beyond simple memorization of anatomical points. They must visualize the three-dimensional relationship between musculoskeletal structures. This is where the specific education provided in remedial courses becomes essential. It shifts the focus from general relaxation to targeted rehabilitation.
Moving Beyond Relaxation: The Remedial Difference
General massage often prioritizes the parasympathetic nervous system response—relaxation. While valuable, this approach often fails to resolve mechanical dysfunctions. In contrast, massage therapy grounded in remedial principles operates on a logic of assessment and correction. Students in our program learn that “remedial” implies a remedy; it is a solution-oriented modality designed to reverse dysfunction and restore range of motion.
When a client presents with hypertonicity, a remedial perspective questions why the tension exists. Is it a result of posture or a shortened muscle group? This analytical process distinguishes a massage therapist who merely relieves stress from one who resolves the physiological drivers of that stress.
The Role of Assessments in Injury Prevention
Treatment without assessment is merely guessing. Effective injury prevention relies on the ability to detect potential failures in the kinetic chain before they manifest as acute pain. During training, we emphasize Dynamic Postural Assessment. This involves observing a client not just statically, but in motion.
For example, a valgus collapse at the knee often indicates weakness in the gluteus medius. If left unaddressed, this increases shear force on the knee joint. A therapist trained in remedial assessments creates a treatment plan that targets these specific imbalances. Consequently, the therapy session becomes a proactive measure against future injuries, ensuring better long-term health and fitness for the client.
Managing Chronic Conditions and Pain
Chronic conditions such as frozen shoulder or sciatica are rarely the result of a single event. They are usually the accumulation of micro-traumas. Addressing these issues requires a strategic approach that goes beyond basic massage.
Consider “Lower Crossed Syndrome.” This involves tight hip flexors and weak glutes. A standard approach might only massage the sore lower back, providing temporary relief. However, the tight hip flexors will immediately pull the pelvis back into an anterior tilt once the client stands up. Remedial training teaches the therapist to release the antagonist muscles to allow the glutes to fire correctly. As a result, the ability to manage pain effectively hinges on this understanding of biomechanics.
Optimizing Athletic Recovery and Performance
In the world of competitive sports, recovery is as important as training. Athletic recovery strategies in remedial massage focus on flushing lactate and preventing adhesion formation.
When working with an athlete, we often focus on deep fascial compartments to prevent entrapment of nerves. This specialized care supports the athlete’s performance by ensuring their mechanical components are operating without restriction. Furthermore, knowing their body is being fine-tuned by a professional provides significant mental benefits and can help lower stress levels before competition.
Advanced Massage Techniques and Career Growth
The toolbox of a remedial therapist is diverse. Remedial training introduces advanced massage techniques like Myofascial Release (MFR) and Muscle Energy Technique (MET). We use MET to lengthen shortened muscles and mobilize restricted joints by having the client actively contract against a counter-force.
Mastering these techniques requires dedication to continuous education. Graduates with a diploma in remedial massage find themselves in high demand. The career opportunities extend to sports teams, physiotherapy clinics, and rehabilitation centers. The market recognizes that a therapist who can perform an orthopedic assessment is a vital asset.
Summary of Core Competencies
The benefits of this specialized training are tangible. To summarize the core skills gained:
- Advanced Assessment: Analyzing posture and gait to identify the root cause of dysfunction.
- Anatomical Fluency: Deep understanding of origin, insertion, and action of major muscle groups.
- Technique Diversity: Proficiency in MFR, MET, and Trigger Point therapy.
- Clinical Reasoning: Designing massage courses of treatment based on logic rather than routine.
Choosing to specialize in remedial work is a commitment to excellence. It demands more study and practice, but the rewards are clear. Whether helping an athlete return to their sport or helping a client move without pain, the ability to assess, reason, and treat effectively is the true value of remedial massage.
The Role of Fascia in Orthopedic Massage: A Clinical Overview
Beyond Muscle: The Fascia Network
Many therapists mistakenly view fascia as merely inert packing material that separates muscles, overlooking its critical role in the broader kinetic chain. They treat the body as a series of isolated levers – biceps flex the elbow, hamstrings flex the knee – and assume that pain is always local to the injury. However, this reductionist view fails to account for the reality of bio-tensegrity. In my experience, ignoring the connective tissue web that links these levers leads to treatment plateaus, where skeletal muscle releases are temporary because the surrounding fascial tension remains unaddressed. Overcoming these plateaus requires the clinical strategies we apply in RSM's Orthopedic Massage Course.
Fascia is the ubiquitous biological fabric that holds us together. While early anatomy texts often discarded this material, modern sports medicine recognizes it as a critical component of biomechanics. This connective tissue forms a continuous web enveloping every bone, nerve, and vessel. Fascia fibers are composed of collagen and elastin, designed to stretch and recoil. However, trauma or inflammation can cause these fibers to disorganize. As a result, fascial layers adhere to one another, restricting the sliding mechanism required for healthy motion.
The Role of Force Transmission and Myofascial Mechanics
To treat orthopedic conditions effectively, a therapist must understand how energy moves through the body. Standard anatomical models often depict muscles as independent pulleys. This is a simplification. In reality, force transmission occurs significantly through the fascial network.
When a muscle contracts, it transmits a significant portion of its energy laterally into the surrounding envelopes. This is known as myofascial force transmission. If the fascial system is healthy, this force distributes evenly. Conversely, if there are fascial restrictions, the load transfer becomes dysfunctional. A restriction in the lumbar fascia can inhibit the glutes, forcing the lower back to compensate. Consequently, this mechanical inefficiency leads to chronic pain. By understanding these connections, we see why treating the site of pain is often insufficient.
Integrating Massage Therapy for Structural Correction
Recognizing the interconnected nature of the body changes how we approach treatment. in orthopedic massage, our goal is the restoration of functional capacity. Massage therapy serves as a mechanical input that physically manipulates the tissue matrix.
When we apply specific fascia massage techniques, we use shear force to melt the ground substance; the fluid component of fascia. Heat and pressure make this substance more fluid, restoring the glide between layers. As the tissue becomes pliable, the tension on pain-sensitive structures decreases. This differs from standard massage. Muscle kneading focuses on blood flow, whereas fascial work requires a slower, deeper engagement to release the tissue barrier.
Advanced Myofascial Approaches
Advanced practitioners integrate myofascial release strategies to address complex patterns. Myofascial pain often presents as referred pain: discomfort felt distally from the source. Trigger points within the tissue cause the fascia to shorten, creating a pull that distorts posture.
Myofascial release therapy aims to disengage these holding patterns. By applying sustained pressure, we encourage the tissue to elongate. This reduces the tension on the skeletal framework, allowing joints to return to neutral alignment so movement becomes efficient again. We often combine this with active motion. For instance, pinning a restricted area while the client moves forces the fascial tissues to slide against the muscle, breaking down adhesions more effectively than passive pressure.
The Role of Therapy in Recovery
The recovery process for athletes relies heavily on the health of their fascia. Many overuse injuries are issues of the fascial system, not just the muscle. Physical therapy protocols often include strengthening exercises. However, strengthening a dysfunction reinforces it. If we load a tissue that is adhered, we create a stronger compensation pattern.
Therefore, manual therapy plays a prerequisite role in rehabilitation. We must restore tissue quality first. Once the myofascial lines are clear, strengthening exercises become effective. At RSM International Academy, we teach that myofascial release is fundamental. Whether for athletic recovery or pain management, acknowledging the continuity of the fascia allows us to deliver more precise and effective therapy.
Common Trigger Points in the Body: A Sports Medicine Perspective
The Physiology of a Trigger Point
At RSM International Academy, we emphasize that one of the most critical distinctions a sports medicine therapist must make is between the site of symptoms and the actual source of dysfunction. Frequently, this source is a trigger point: a localized physiological crisis occurring deep within the muscle fibers.
A myofascial trigger point is clinically defined as a hyperirritable spot located within a taut band of skeletal muscle. Under microscopic analysis, this phenomenon represents a metabolic deadlock. The sarcomeres, the contractile units of the tissue, become locked in a state of sustained contraction. This continuous engagement consumes energy and creates mechanical compression on local capillaries. Consequently, the area suffers from ischemia (oxygen deprivation) and an accumulation of metabolic waste products. This acidic chemical environment sensitizes nociceptors, creating the intense tenderness identified during palpation.
When we strum this taut band perpendicularly, we often elicit a local twitch response. This transient contraction is a spinal reflex, confirming that we have located the precise epicenter of the pathology. However, as we teach in RSM's Trigger Point Therapy Course, not all points behave the same way. We must differentiate between the active trigger and the latent trigger.
Active vs. Latent Trigger Points
An active trigger is the immediate cause of a patient’s complaint. It produces pain spontaneously, during movement, or at rest. It is the primary reason clients seek treatment. In contrast, a latent trigger does not produce spontaneous pain; it is only tender when compressed.
While a latent trigger may appear less urgent, it is often the silent architect of restricted range of motion and muscle weakness. If left unaddressed, mechanical stress or fatigue can easily convert a latent point into a painful trigger, precipitating an acute myofascial pain syndrome.
Referred Pain and Key Locations
The most confounding aspect of myofascial pain for patients is the displacement of symptoms. Referred pain occurs because nociceptive signals from the trigger converge on the same spinal neurons as signals from other bodily regions. The brain, unable to isolate the exact source, projects the sensation to a predictable somatic reference zone. Understanding these maps is essential for effective massage and rehabilitation.
Upper Body: The Neck and Trapezius
In modern clinical practice, upper body tension is ubiquitous due to poor posture and ergonomic stressors. The Upper Trapezius is the most frequent site for tender points. A trigger here typically refers pain up the posterolateral aspect of the neck and into the temple, causing tension headaches.
Similarly, the Sternocleidomastoid (SCM) is a critical, yet often overlooked, structure. Located in the anterior neck, trigger points in the SCM can refer pain deep into the ear, across the cheek, or above the eye. Because these symptoms mimic sinus issues or ear infections, the muscular origin is frequently missed.
Lower Body: The Back and Pelvis
In the lower body, the Quadratus Lumborum (QL) is a primary villain in low back pain. This stabilizer connects the pelvis to the lumbar spine. When an active trigger develops in the QL, it refers pain to the sacroiliac joint and the lower buttock. Crucially, this can create a “fake” hip pain or a functional leg length discrepancy, altering the kinetic chain and leading to compensatory injuries in the knees or ankles.
Deeper in the hip, the Gluteus Minimus acts as a mimic for sciatica. Its referred pain travels down the leg, closely resembling nerve root compression. Unlike true sciatica, however, there are no neurological deficits. In complex cases of myofascial pelvic pain, therapists must also evaluate the deep rotators and pelvic floor, as tension here can manifest as groin or coccyx discomfort.
Treatment Strategies for Myofascial Pain
Resolving myofascial trigger points requires a strategy that goes beyond simple pressure. The goal of treatment is to unlock the sarcomeres and restore perfusion to the starved tissue.
Manual release techniques, such as ischemic compression and deep tissue massage, are foundational. By applying sustained pressure to the spot, we temporarily occlude blood flow. Upon release, fresh, oxygenated blood floods the area, flushing out inflammatory chemicals. This must be followed by stretching to reset the resting length of the muscle.
In cases where chronic issues resist manual therapy, injection therapy may be necessary. Trigger point injections (or dry needling) involve inserting a needle directly into the taut band. This mechanical disruption destroys the dysfunctional motor endplate activity, allowing the muscle to reset.
Ultimately, successful therapy requires identifying perpetuating factors. Whether the cause is skeletal asymmetry, nutritional deficiency, or ergonomic stress, the treatment must address the root. By mapping locations and understanding the mechanism of referred symptoms, we move beyond symptom management and towards true structural correction.
Choosing the Best Textbooks for Massage Therapy
At RSM we aim to raise the level of massage therapists, and one of the ways we do this is to remember that hands do not heal what the mind does not understand. In my years of clinical practice and teaching sports medicine-based modalities, I have observed that a therapist’s effectiveness is directly proportional to their theoretical grasp of the human machine. When a student relies solely on intuition without anatomical precision, their results hit a ceiling. However, when they ground their practice in evidence-based literature, they gain the ability to troubleshoot complex kinetic chain dysfunctions.
Building a library of books is not merely an academic exercise; it is the construction of a diagnostic toolkit. The right resources bridge the gap between abstract theory and practical application. This transition is the core focus of our Remedial Massage Course. These materials transform a two-dimensional image of a muscle into a three-dimensional understanding of tension, torque, and force transmission. Below, I outline the essential reading materials that have defined my curriculum and clinical approach.
Foundational Anatomy for Massage Therapy
Before a student can treat dysfunction, they must master structure. Anatomy is the map; without it, you are navigating blind. Many generic programs rush this phase, leading to graduates who can perform a sequence but cannot locate a specific attachment site. This lack of precision results in generic rubbing rather than targeted therapy.
Trail Guide to the Body by Andrew Biel remains the gold standard student resource for surface palpation. Its value lies not in dense medical jargon, but in its navigational logic. Biel treats the body as a landscape to be explored, providing specific landmarks that allow manual therapists to orient themselves with absolute certainty.
When I teach palpation, I emphasize that locating a muscle belly is insufficient. One must distinguish the fiber direction, the exact musculotendinous junction, and the subtle texture changes that indicate hypertonicity. Biel’s guide excels here because it forces the reader to visualize structures through the skin. This visualization leads to better tactile sensitivity. If you cannot visualize the deep external rotators underneath the gluteus maximus, you cannot effectively treat piriformis syndrome. You are simply guessing depth. Learning to palpate with this level of specificity allows you to differentiate between a taut band of muscle and a nerve entrapment.
A Guide to Clinical Massage Techniques
Once structure is understood, the focus shifts to pathology and treatment. Clinical massage requires a deviation from relaxation protocols. It demands a systematic approach to restoring function. For this, Clinical Massage Therapy: Understanding, Assessing and Treating Over 70 Conditions by Rattray and Ludwig is indispensable.
This text aligns closely with the sports medicine philosophy we uphold at RSM. It does not view massage as a vague holistic remedy but as a mechanical intervention for specific physiological problems. The authors structure the information by condition – whiplash, tendinitis, frozen shoulder – rather than just body part. This causal approach is critical. For instance, when treating lateral epicondylitis (tennis elbow), simply rubbing the elbow is rarely effective. The book explains how proximal restriction in the shoulder or cervical spine often contributes to the distal symptom.
By studying this text, therapists learn to design treatment plans based on the stage of healing. Treating an acute injury with deep friction can exacerbate inflammation; conversely, treating chronic fibrosis with light effleurage accomplishes nothing. Rattray and Ludwig provide the insights necessary to match the intensity of the technique to the pathology of the tissue. This reduces the risk of over-treating a sensitive area or under-treating a stubborn adhesion.
The Definitive Book on Fascial Lines
Standard anatomy texts often present muscles as isolated units (biceps, triceps, quadriceps) separated by clear boundaries. In reality, the body functions as a continuous tensegrity network. Thomas Myers’ Anatomy Trains revolutionized how we perceive movement. It moves beyond single-muscle theory and introduces the concept of myofascial meridians.
For the sports medicine therapist, this functional anatomy perspective is vital. I frequently see clients presenting with plantar fasciitis who have failed to respond to local foot treatments. Using the logic found in Myers’ work, we can trace the Superficial Back Line and often find the root tension in the hamstrings or the suboccipital region. When the therapist releases the calf and hamstring, the tension on the plantar fascia drops.
This text helps learners see the “ghost in the machine.” It explains why a forward head posture creates tension in the lower back and how a rotation in the pelvis affects the arch of the foot. Integrating these concepts allows you to treat the pattern, not just the pain. Reading this text requires patience, as the concepts challenge traditional education, but the clinical payoff is significant. It turns a localized treatment into a structural integration session.
Understanding Pain and Dysfunction
Pain is rarely where the problem is. This is a mantra I repeat constantly. The most sophisticated resource for understanding referred pain patterns is Myofascial Pain and Dysfunction: The Trigger Point Manual by Travell and Simons. This two-volume set is arguably the most important work in the history of soft tissue therapy.
Travell and Simons mapped the referred pain patterns of skeletal muscles with rigorous detail. They demonstrated that a headache above the eye often originates from the sternocleidomastoid, and that “sciatica” is frequently a referral from the gluteus minimus. Without this knowledge, a practitioner chases symptoms. They rub the temple for the headache or the leg for the sciatica, achieving only temporary relief because the generator of the signal remains untouched.
Mastering this material elevates a therapist from a relaxation provider to a pain management specialist. It provides the causal link between a hidden knot in muscle A and the debilitating symptom in area B. While the text is dense, it serves as an ultimate reference. When a client presents with a symptom that defies logic, checking the referral maps in this book usually provides the answer.
Moving Beyond the Basic Therapy Curriculum
To truly enhance your practice, you must eventually step outside the realm of pure massage texts and venture into orthopedic assessment. Massage therapists who wish to work with athletes must speak the language of physical therapists and osteopaths. Orthopedic Physical Assessment by David Magee is a cornerstone for this transition.
While not strictly a massage book, it teaches the special tests required to rule out structural damage. If a client presents with shoulder pain, how do you know if it is a rotator cuff tear or simple supraspinatus tendonitis? Magee’s text provides the testing protocols. Knowing when not to treat is just as important as knowing how to treat. If a client tests positive for a structural tear, the responsible action is referral, not massage. This diagnostic capability builds immense trust with clients and other medical professionals.
This level of applied anatomy fosters critical thinking. It moves the practitioner away from routine sequences and toward hypothesis-driven treatment. You assess, you treat, you re-assess. If the movement marker does not improve, you adjust your strategy. This cycle of clinical reasoning is what we strive to instill at RSM, and these texts provide the intellectual foundation for that process.
Essential Reading List
To summarize, building a library is an investment in your career longevity. The following resources provide a comprehensive blend of technique, anatomy, and pathology:
- Trail Guide to the Body (Andrew Biel): The non-negotiable prerequisite for surface anatomy and palpation skills.
- Clinical Massage Therapy (Rattray & Ludwig): The blueprint for treating specific pathologies and understanding the stages of healing.
- Anatomy Trains (Thomas Myers): The key to understanding fascial lines and kinetic chain relationships.
- Myofascial Pain and Dysfunction (Travell & Simons): The encyclopedic guide to trigger points and referred pain patterns.
- Orthopedic Physical Assessment (David Magee): The bridge between soft tissue therapy and medical diagnosis.
These volumes do not sit on a shelf to look impressive; they are working documents. A ragged, highlighted, and coffee-stained book indicates a therapist who is constantly refining their understanding. As specific protocols evolve, the underlying anatomy remains constant. Therefore, a deep investment in these texts ensures that your practice remains built on solid ground, regardless of passing trends in the wellness industry.
By integrating the logic from these texts, connecting the kinetic chain, respecting referral patterns, and understanding tissue pathology, we elevate the profession. We move from being technicians who follow a routine to clinicians who solve problems. That is the standard we aim for, and it begins with what you read.
An Introduction to Orthopedic Assessment Skills
In the specialized field of sports medicine-based massage, the distinction between a relaxation therapist and a clinical practitioner is defined by the accuracy of their evaluation. If we fail to understand the biomechanical cause of a client’s complaint, we are merely chasing symptoms rather than resolving the root dysfunction. This limited approach leads to temporary relief and often allows the underlying issue to worsen.
To evolve from a technician into a clinician, one must adopt a rigorous mindset. We must view the body not just as tissues to be manipulated, but as a complex, interconnected musculoskeletal system where every pain pattern tells a logical story. This article outlines the fundamental framework required to master this transition. These principles are what students put into practice throughout RSM's Orthopedic Massage Course.
Decoding the Orthopaedic History
True clinical competency begins before the client ever reaches the treatment table. It starts with the subjective interview, which is the most critical tool in our diagnostic arsenal. Collecting a comprehensive orthopaedic history allows us to narrow down the differential diagnosis significantly.
We must ask targeted questions to understand the mechanism of injury. Did the pain start suddenly after a specific movement, or was it an insidious onset over months? These details provide vital clues about the tissues involved. For instance, deep, aching sensations often originate from a bone or joint capsule, whereas sharp, shooting sensations typically implicate nerve entrapment.
This investigation into the clinical presentation guides our expectations. By listening to how the symptoms behave, whether they improve with movement or worsen with rest, we can predict the underlying physiology and mechanical faults we will encounter.
Navigating Anatomy and the History Physical
Once the history is established, we move to the physical examination. This transition relies on the “history physical” connection, the bridge between what the client reports and what the therapist detects. To cross this bridge effectively, a deep working knowledge of anatomy is non-negotiable.
Palpation is a primary skill here, but it must be performed with specific intent. We are not just searching for “knots”; we are assessing palpation length and tissue texture. For example, if a muscle feels short and tight, we must determine if this is true adaptive shortening or a protective spasm due to instability elsewhere. We trace nerve pathways and identify trigger points that reproduce the “familiar pain.” This reproduction confirms that we have located the source of the problem.
Assessment of Joint Function
A key component of the physical exam is evaluating joint mechanics. We assess both active and passive range of motion (ROM) to isolate the limiting factor.
- Active ROM: Tests the ability of the muscle to generate force and the client’s willingness to move.
- Passive ROM: Tests the integrity of the inert structures: ligaments and the joints themselves.
If a client has full passive range but limited active range, the issue is likely muscular weakness or neurological inhibition. Conversely, if both active and passive ranges are restricted, we suspect a capsular pattern or bony obstruction. During these assessments, we watch closely for deviations in joint movement, such as a hitch during knee flexion or winging of the scapula. These subtle cues reveal the breakdown in kinetic chain function.
Special Tests and Strength Testing
When basic motion and palpation do not provide a definitive answer, we utilize special tests. These are specific maneuvers designed to stress particular tissues to see if they elicit a positive sign.
For instance, to assess cervical radiculopathy, we might employ a compression test like Spurling’s Maneuver. By applying a controlled axial load, we narrow the neural foramen. If this action reproduces the arm pain, it indicates nerve root irritation. Similarly, strength testing helps us distinguish between tendon pathology and neurological weakness. A single test is rarely diagnostic on its own. However, when we combine a positive special test with specific history findings, our confidence in the assessment increases. This data triangulation separates a medical grade assessment from a simple guess.
Identifying Red Flags: Fractures and Surgery
A crucial aspect of orthopedic assessment is knowing when not to treat. As sports therapists, we operate within a specific scope, and it is our responsibility to identify “red flags” that require immediate referral.
We must be vigilant for signs of fractures, systemic disease, or conditions that require surgery. If a client presents with unremitting night pain, unexplained weight loss, or severe deformity following trauma, manual therapy is contraindicated. In these cases, the correct treatment is a referral for imaging or a consultation with a specialist. Recognizing these limits protects the client and defines the professional boundaries of our practice.
The Path to Mastery
Developing high-level assessment skills requires a commitment to logic and precision. By mastering the H.O.P.S. protocol (History, Observation, Palpation, Special Tests) and understanding the biomechanics of compression and tension, you elevate your practice. The goal is to identify the length and tension relationships that drive dysfunction. This rigorous approach ensures that we do not just treat pain temporarily, but help restore function permanently.
Essential Anatomy for Massage Therapists: The Clinical Foundation
For a massage therapist, deep anatomical fluency determines the difference between a simple relaxation session and an intervention that resolves chronic pain. When I observe students in our Trigger Point Therapy Course initially grappling with musculoskeletal structures, I often notice a tendency to view muscles in isolation. However, the body functions as an interconnected kinetic chain.
Effective treatment requires seeing these connections. A pain signal in the knee often originates from hip dysfunction. Similarly, numbness in the fingers frequently begins with entrapment in the cervical spine. Mastering this logic allows a massage therapist to treat causes rather than just symptoms. This level of knowledge separates the elite practitioner from the hobbyist.
Defining the Standard for Massage Therapists
In sports medicine, precision is non-negotiable. A general understanding of where a muscle starts and ends fails to account for the complex interplay of fascia, nerve pathways, and biomechanical levers. Massage therapists who wish to excel must adopt a three-dimensional view of the body.
For instance, consider the anatomical position. This standard reference point is critical for describing location and movement. Without it, clinical notes become ambiguous, and communication with other healthcare professionals breaks down. If a therapist cannot accurately describe a lesion relative to the midline, their professional credibility diminishes. Consequently, anatomy becomes the bridge between intuitive touch and medical science.
The Layered Reality of Muscle Anatomy
When palpating the body, the first challenge is distinguishing between superficial and deep layers. The deltoid muscle, for example, forms the rounded contour of the shoulder and is a powerful mover. Because it is superficial, it is easily accessible. However, treating the deltoid alone rarely solves shoulder pathology. The true drivers of dysfunction often lie beneath it in the rotator cuff. Ignoring these deep layers leads to incomplete treatment.
To break the cycle of recurring pain, one must understand muscle anatomy as a system of layers. Consider the sternocleidomastoid muscle (SCM) in the anterior neck. This prominent muscle is a frequent source of trigger points that mimic tension headaches. Because the SCM overlays the major vessels of the neck, deep work here requires extreme caution. A skilled practitioner knows exactly how to manipulate the muscle belly safely, a technique that relies entirely on a detailed mental map of the cervical region.
Precision Treatment and Client Outcomes
The upper extremity offers a clear example of how detailed anatomical knowledge improves clinical outcomes. Many clients present with lateral or medial elbow pain. A basic massage therapy approach might involve rubbing the painful spot. A sports medicine approach, however, traces the pain to its mechanical origin.
Pain at the lateral epicondyle typically stems from the extensor group of the forearm. Overuse of the extensor digitorum creates constant traction on the common extensor tendon. Friction massage at the attachment site helps, but releasing the muscle bellies in the forearm provides lasting relief.
Conversely, pain at the medial epicondyle involves the flexor group. Here, the flexor carpi radialis and ulnaris are the usual suspects. Tightness in these muscles pulls on the medial humerus, causing inflammation. We must also look at the brachioradialis muscle. This muscle acts as a bridge between the upper arm and the forearm. Because of its leverage, it often harbors significant tension.
This detailed breakdown of the upper limb demonstrates why specific training is vital. If you can explain to a client that their elbow pain is a result of wrist mechanics, you build immense trust.
Why a Sports Medicine Program Demands More
At RSM, our curriculum integrates functional anatomy with clinical technique. A standard massage therapy course might ask you to name the quadriceps. Our approach asks you to analyze how those muscles affect pelvic tilt and lumbar stability.
This depth of understanding transforms the way you work. You stop chasing pain and start correcting dysfunction. For aspiring therapists, investing in a rigorous education is the most important career decision they will make. Schools that gloss over these complexities do their graduates a disservice.
- Assessment: Identifying bony landmarks.
- Hypothesis: Connecting pain to specific structures.
- Treatment: Applying precise techniques.
I believe the future of our industry lies in this level of integration. To succeed, you must be willing to study the flexor carpi, the extensor digitorum, and the medial epicondyle not just as words, but as tangible structures. Expanding your anatomical knowledge expands your potential to help others. This is the essence of a successful career in sports medicine.
The Value of Sports Massage for Amateur Athletes
In my time at RSM International Academy, one critical difference I’ve observed between professional and amateur athletes is that professionals treat recovery as a mandatory component of their job. Amateurs, on the other hand, often view it as optional. This mindset creates a dangerous physiological gap. The amateur athlete pushes their body with high intensity while managing work and family, yet rarely affords their musculoskeletal system the downtime required to repair. As a result, cumulative load leads to chronic restriction, altered biomechanics, and eventually, injury.
Defining the Scope of Sports Massage
It is a common misconception that sports massage is simply a vigorous spa treatment. In RSM's Sports Massage Course, I teach students that massage is a mechanical intervention designed to manipulate soft tissue to achieve specific physiological outcomes. Unlike relaxation modalities, the goal is to restore functional tissue length and optimize the sliding surfaces between fascial layers.
When we treat an athlete, we view the body as a kinetic chain. A restriction in the calf muscles, for instance, reduces ankle dorsiflexion. This limitation forces the knee to compensate during movement, altering the load on the patellar tendon. Consequently, therapy applied to the calf is a strategic maneuver to protect the knee. This clinical reasoning defines sports massage therapy; we identify the root cause of dysfunction rather than merely chasing symptoms.
The benefits of this approach are tangible. By targeting muscles shortened by repetitive strain, we restore range of motion. This allows the athlete to train with proper mechanics, reducing the risk of compensatory patterns that lead to acute failure.
Addressing Muscle Tension and Hypoxia
To understand the efficacy of massage, one must understand muscle tension at a microscopic level. When an athlete trains to failure, ATP (adenosine triphosphate) depletion can cause myosin heads to lock onto actin filaments, forming a “rigor complex.” When these complexes accumulate, they manifest as palpable knots. This tension compresses local capillaries, restricting blood flow and creating a hypoxic (low oxygen) environment.
Sports massage interventions mechanically disrupt this cycle. By applying direct compression, the therapist forces a local hyperemia – an influx of fresh, oxygenated blood – into the tissue. This flush brings the nutrients necessary to break the chemical bond, allowing the muscle fibers to relax. Pain signals are subsequently dampened as metabolic byproducts are cleared by the lymphatic system.
There is often confusion regarding deep-tissue massage versus sports specific work. While deep-tissue massage focuses on accessing sub-layers of musculature to release chronic holding patterns, sports massage is outcome-specific. Tissue massage in a sports context varies based on the training cycle. During heavy training blocks, we use myofascial release to unglue adherent layers. Conversely, pre-event techniques are stimulating to prime the nervous system.
The Strategic Value of Maintenance Massage
For the amateur, consistency is the hardest variable to master. Maintenance massage serves as a scheduled audit of the body. Regular sessions allow the therapist to detect muscular imbalances before they evolve into debilitating injuries.
We frequently see runners develop plantar fasciitis. Often, the precursor, tightness in the gastrocnemius and soleus, was present for months. A consistent maintenance massage schedule identifies this hypertonicity early. By releasing the calf muscles and improving the flexibility of the posterior chain, we relieve tension on the plantar fascia before inflammation sets in.
This preventative approach is where massage yields the highest return. It is far easier to reduce tension in an overworked muscle than to rehabilitate a torn one. Injuries derail training progress, leading to deconditioning. Regular therapy keeps the tissue compliant and resilient, capable of handling progressive overload.
Enhancing Recovery and Sports Performance
The timing of massage relative to training is critical. Post-workout massage focuses on shifting the body from a sympathetic (fight or flight) state to a parasympathetic (rest and digest) state. After high-intensity sports activity, the body is flooded with cortisol. Until these levels drop, deep restorative processes cannot begin.
Massage facilitates this neurological shift. The rhythmic application of pressure lowers heart rate and accelerates the clearance of metabolic waste. While massage cannot “cure” Delayed Onset Muscle Soreness (DOMS), it significantly reduces the perception of pain, improving mobility during the healing phase.
Ultimately, the goal is to improve performance. Massage achieves this by increasing the compliance of the musculotendinous unit. A compliant muscle stores and releases elastic energy more efficiently than a stiff one, translating to better power production. Furthermore, specific sports massage techniques aid proprioception. When fascia is restricted, sensory feedback to the brain is dulled. By freeing these restrictions, we enhance the athlete’s awareness of joint position and technique.
Key Benefits of Pre and Post-Workout Massage
- Accelerated Recovery: Massage therapy speeds up the clearance of metabolic waste and reduces the duration of DOMS, allowing for more frequent high-quality training.
- Injury Prevention: Regular assessment identifies and corrects muscular imbalances and soft tissue restrictions before they result in acute injury.
- Functional Flexibility: Massage restores normal muscle length and fascial glide, ensuring functional range of motion is maintained under load.
- Psychological Focus: Therapy reduces sympathetic nervous system dominance, lowering anxiety and promoting a mindset conducive to high-level performance.
At RSM International Academy, we teach that sports massage is a dialogue with the nervous system. Whether preparing for a marathon or simply trying to stay active, integrating massage into the routine is a decision that pays dividends in longevity. Sports massage for amateur athletes is not a luxury; it is a fundamental pillar of athletic health.