RSM Blog: Sports Medicine and Massage Insights
A Review of Cases Where Trigger Point Therapy Helps
We often encounter patients who point to a specific spot on their shoulder or back and say, “The pain is right here.” They press into the muscle, describing a sensation that feels like a deep bruise or a tight knot. In RSM’s Trigger Point Therapy Course students learn to recognize this immediately as the hallmark of a myofascial dysfunction. It requires more than just general relaxation to resolve. It needs precision.
Pain is rarely as simple as it appears on the surface. The “knot” the patient feels is a palpable nodule within a taut band of skeletal muscle, known technically as a trigger point. These hypersensitive spots cause localized tenderness, but their most deceptive trait is their ability to project sensation to distant areas. Understanding the specific scenarios where this modality is effective is crucial for any serious therapist. Whether you are a physiotherapist, a sports medicine professional, or a massage therapist looking to elevate your practice, recognizing the indications for this treatment is the first step toward resolving complex pain syndrome issues.
Defining the Myofascial Trigger Point
To understand why we treat these points, we must first understand what they are physiologically. A myofascial trigger point is not merely a “tight muscle.” It is a localized area of hypoxia and metabolic crisis. Under the microscope, we observe that a specific cluster of sarcomeres – the basic contractile units of muscle fiber – has become locked in a state of continuous contraction.
This sustained contraction compresses local capillaries, restricting blood flow. Without adequate circulation, the tissue cannot receive oxygen or flush out metabolic waste products like lactic acid. This creates a chemical environment that sensitizes nociceptors, creating a feedback loop of contraction and ischemia. The result is a distinct, palpable nodule. When stimulated, this nodule often produces a “twitch response,” a reliable diagnostic sign distinguishing a true trigger point from general muscle tension.
We distinguish between active and latent points. An active point causes spontaneous pain even when the muscle is at rest. A latent point does not cause spontaneous pain but restricts movement and causes weakness. Latent points can persist for years, silently altering movement patterns until a sudden overload activates them, resulting in an acute episode of muscle pain.
Mechanisms of Referred Pain and Muscle Pain
The most perplexing aspect of myofascial pain for patients is referred pain. This occurs when nociceptive signals from the trigger point converge with signals from other areas of the body in the spinal cord. The brain interprets the pain as coming from the area where the nerves converge rather than the source of the pathology.
For example, a patient may complain of a deep ache in their wrist. A novice might focus on the forearm or carpal tunnel. However, an experienced clinician understands that a trigger point in the scalene muscles of the neck can refer pain directly down the arm to the thumb. Treating the wrist provides zero relief because the driver is in the cervical region.
This referral mechanism is why accurate diagnosis is paramount. We cannot simply chase the pain. We must map it. Successful therapy relies on a deep knowledge of these patterns combined with tactile sensitivity.
Clinical Approaches to Back Pain
Low back pain is one of the most common complaints in clinical practice and is frequently misdiagnosed. While spinal pathologies exist, a significant volume of chronic back pain is myofascial in origin.
The Quadratus Lumborum (QL) is a primary suspect. This deep abdominal muscle connects the pelvis to the spine. When trigger points develop here, the pain is often described as a paralyzing ache in the lower back that can mimic nerve root compression.
We also see significant involvement of the gluteus medius and minimus. A trigger point in the gluteus minimus can refer pain down the posterior thigh, mimicking sciatica. We call this “pseudo-sciatica.” Unlike true sciatica caused by nerve compression, this condition is caused by a muscular referral pattern. The solution is not injections or surgery; it is precise manual therapy applied to the gluteal muscles to release the contraction.
In these instances, applying general pressure is insufficient. The therapist must apply ischemic compression – sustained pressure that temporarily restricts blood flow to the knot. When released, a rush of fresh blood floods the tissue, helping to break the metabolic crisis.
Beyond Basic Trigger Point Massage
While manual compression is the foundation, we must distinguish between relaxation massage and clinical trigger point massage. In a sports medicine context, the goal is functional restoration, not just parasympathetic activation.
This specific type of massage therapy requires constant communication. We use a pain scale to ensure pressure remains within a “therapeutic discomfort” range. If the pressure is too light, we fail to induce physiological change. If it is too aggressive, the patient’s body creates a protective guarding response, tightening the muscle further.
We often utilize “stripping,” applying deep, slow gliding pressure along the taut band to elongate sarcomeres. Furthermore, we must address the fascia. Myofascial release is often used in conjunction with trigger point work. If the fascia is adhered, it perpetuates the formation of new muscle knots. By mobilizing the fascia, we create the space necessary for the muscle to function correctly.
Therapy Integration in Sports Medicine
In the athletic population, trigger point therapy serves a vital role in performance enhancement. Athletes subject their bodies to repetitive high-force loads, leading to micro-trauma and the formation of latent trigger points.
Consider the overhead athlete. The infraspinatus muscle is constantly working to decelerate the arm. It is common to find trigger points here that refer pain deep into the shoulder joint. An athlete might suspect a structural impingement, but the true culprit is the posterior shoulder musculature. By identifying and treating these points early, we restore elasticity and contractility. A muscle plagued by knots is a weak muscle; releasing them improves power output.
This approach is not limited to manual techniques. Some practitioners utilize dry needling, inserting a thin needle directly into the point. This mechanical stimulus elicits a twitch response that rapidly resets the neurological feedback loop. While manual therapy is our focus at RSM, dry needling is a potent adjunctive tool in sports medicine. In medical settings, doctors may even use trigger point injections or point injections with anesthetic, though manual release is often equally effective for long-term management.
Strategies for Chronic Pain Management
Chronic pain conditions like myofascial pain syndrome present a unique challenge. The nervous system becomes sensitized, and the pain is no longer just about the tissue. However, managing peripheral input remains essential. Trigger points serve as constant sources of nociceptive input that bombard the central nervous system. By reducing the number of active points, we lower the overall “noise” the system must process.
Headaches are a prevalent form of chronic pain where this approach excels. Tension-type headache patterns are overwhelmingly muscular. The upper trapezius and sternocleidomastoid (SCM) are usual suspects. The SCM is notorious for causing dizziness and pain wrapping around the eye. A patient may have seen specialists with no clear diagnosis, only to find pain relief when a skilled therapist releases the SCM.
Case Studies in Extremities
Specific extremity cases demonstrate where this targeted point therapy is most effective.
- Lateral Epicondylitis (Tennis Elbow):
Often diagnosed as a tendon issue, the pain is frequently exacerbated by trigger points in the Supinator and Extensor Carpi Radialis Longus. Releasing the muscle belly relieves tension at the attachment site. - Plantar Fasciitis:
Pain in the heel is often driven by tightness in the calf muscles. A trigger point in the gastrocnemius refers pain directly to the foot arch. We must treat the calf to fix the foot. - Iliotibial (IT) Band Syndrome:
You cannot “release” the IT band by rubbing it. However, treating the Tensor Fasciae Latae (TFL) which tensions it provides relief. Releasing trigger points in the TFL is critical for lateral knee pain.
Achieving Lasting Pain Relief
The ultimate goal of any treatment is lasting correction. If we release a trigger point but the patient returns to the same poor biomechanics, the point will return.
We must act as detectives. Is the patient’s posture comprising their recovery? Are they deficient in essential nutrients? These factors influence the health of the muscle tissue. Education is a form of therapy. We teach patients self-release techniques and prescribe stretching to load the tissue through its full range. A strong, flexible muscle is resistant to muscle knots.
At RSM, we view the body as a tensegrity structure. Whether dealing with an elite athlete or an office worker, the principles remain the same. We locate the metabolic crisis, apply precise force to resolve it, and correct movement patterns to prevent recurrence.
Trigger points are the body’s way of signaling overuse or protection. By listening to these signals and applying targeted therapy, we guide the body back to balance. The effectiveness of this method lies in its specificity. When you reproduce the patient’s exact pain and then melt it away, you engage in a profound form of healing. This is the expertise we pass on to our students. It requires study and practice, but for patients living in pain, it is often the only thing that helps.
Summary of Key Indications
To consolidate this information, here are the primary indications where we find this therapy most beneficial:
- Head and Neck: Tension headaches, migraines, TMJ pain.
- Shoulder and Arm: Rotator cuff mimics, frozen shoulder, carpal tunnel mimics.
- Torso and Back: Chronic pain in the lower back, mechanical spine pain.
- Hip and Leg: Piriformis syndrome, sciatica mimics, plantar fasciitis.
Understanding the muscular origins of these conditions allows us to treat the cause rather than the symptom. It transforms the therapist from a passive provider of comfort into an active agent of recovery.
Mastering Pre Event Sports Massage Techniques
The Physiology of Pre-Event Readiness
The atmosphere of a warm-up area thirty minutes before a competition is distinct. It is charged with anticipation and the physiological noise of bodies priming themselves for exertion. As therapists, we step into this space to facilitate readiness, not to resolve pathology. We are not there to fix long-standing issues; we are there to fine-tune an engine that is already running.
In RSM International Academy’s Sports Massage Course, we emphasize that the objective of any treatment delivered immediately prior to competition is performance optimization. We move away from the sedation typical of relaxation therapies and toward stimulation. We aim to optimize viscoelasticity in the soft tissue and prime the nervous system for reaction. A therapist who treats a sprinter with the slow strokes used for a recovering marathon runner is actively hindering performance.
Our goal is to increase local circulation, which warms the muscle and reduces the viscosity of fluids within the fascial layers. When tissue is cold, it is brittle; when it is warm, it is pliable. We also aim to reset neural tone, achieving “controlled arousal” where muscles are awake and responsive without restricting range of motion.
Timing and Context in Event Massage
The “pre-event” window technically spans 24 hours up to the minute of competition, but the most critical work often happens in a 10 to 15-minute micro-session immediately prior to the start. This timing dictates the tempo. If an athlete is on the table 10 minutes before their start time, the pace must match the urgency of their impending exertion.
This context requires the therapist to be adaptable. You may be working on a patch of grass or a bench, lacking the luxury of perfect ergonomics. Consequently, your body mechanics must be impeccable to deliver effective force without compromising your own posture. The techniques used here differ drastically from clinical work; we prioritize speed, rhythm, and superficial vascularity over depth.
Key Massage Techniques for Event Preparation
The specific modalities we select are designed to wake up the body. We avoid deep tissue sculpting which might cause soreness, focusing instead on rapid, stimulating inputs.
Effleurage and Vascular Flush
Effleurage in this setting is fast and vigorous. We use palms and forearms to create friction, generating a thermal reaction that dilates capillaries. This serves as a vascular flush, mechanically assisting venous return to ensure the local muscle environment is oxygenated. The stroke rate should be approximately 100 to 120 beats per minute, signaling the athlete’s body to upregulate heart rate and respiration.
Tapotement Dynamics
Percussive techniques are iconic in this phase. Tapotement is often used pre-event because of its direct excitatory effect on the nervous system. By striking the body rhythmically, we stimulate mechanoreceptors that detect changes in muscle length. This triggers a stretch reflex, increasing resting tone to make the muscle “springy.”
Effective tapotement massage techniques should be applied with loose wrists to ensure the force penetrates without causing pain. For athletes requiring explosive power, this is essential. It tells the body that high-velocity movement is imminent. However, for an athlete already over-stimulated, we use it sparingly to avoid inducing anxiety.
Compression and Direct Pressure
We utilize direct pressure to address specific areas of hypertonicity that might alter biomechanics. If a gluteal muscle is locked, it may inhibit hip extension. We apply broad, rhythmic compression, pressing into the tissue and releasing to mimic the muscle pump action. This encourages blood flow into the deeper belly of the muscle. If a trigger point is active, static pressure is kept short, to between 10 and 15 seconds, to avoid shutting down power output.
Jostling and Mobilization
Jostling is one of the most effective tools for resetting tone without sedation. This involves grasping the muscle belly or limb and shaking it rhythmically. It confuses proprioceptors in a beneficial way, encouraging a “letting go” of involuntary holding patterns. We combine this with dynamic mobilization, taking joints through their available range of motion to lubricate the capsule with synovial fluid. We ensure the hinge is oiled before the load is applied.
The Nervous System and Event Performance
The interface between the therapist’s hands and the athlete’s body is mediated by the nervous system. Pre-event massage prepares your body physically, but its impact on the autonomic nervous system is equally vital.
We navigate the balance between the sympathetic (fight or flight) and parasympathetic (rest and digest) systems. Standard massage often induces a parasympathetic state, which is detrimental right before a race. We need the athlete in a sympathetic-dominant state that is focused rather than chaotic. By keeping strokes fast and irregular, we facilitate this activation. Conversely, if an athlete is hyper-anxious, we might slow our rhythm slightly to bring them down to a performance state.
Knowing what to avoid is as important as technical proficiency. Pain triggers a guarding response, so we avoid deep friction that could cause micro-trauma. We also avoid prolonged static stretching, as holding a stretch immediately prior to maximal exertion can temporarily dampen power output. Instead, we favor dynamic movement to achieve length.
Adapting Therapy to the Athlete
At RSM, we teach that the requirements of the sport and the individual dictate the therapy. A powerlifter relies on stiffness for stability; loosening them too much may compromise their safety under heavy loads. Their session should focus on heat generation. In contrast, a marathon runner relies on fluid mechanics, requiring free-gliding fascial chains.
The therapist acts as a pillar of stability in the chaotic event environment. Our demeanor is as influential as our hands. We must be calm and professional, adapting to whether the athlete prefers silence to visualize or chatter to dissipate nerves. Hygiene and logistics are also paramount; using too much oil is a rookie error that can prevent an athlete from gripping a ball or racket effectively.
Integrating Pre-Competition Massage Safety
While the focus is performance, a deep understanding of injury and rehabilitation informs our decisions. If an athlete is taping a previous sprain, we work around it. If we detect heat or tension indicating a re-injury risk in a hamstring, we must ethically inform the medical team. This intersection of performance support and medical oversight is where event therapy shines.
The transition from a spa therapist to a sports therapist requires a shift in intent. In sports, physiology dictates pressure, and the goal is function. We manipulate soft tissue to create a specific mechanical and neurological state. It requires a knowledge of anatomy that allows you to visualize the layers under your hands and understand the origin and insertion of muscles.
High-quality event sports massage is an integral part of the athletic puzzle. When executed correctly, it gives the athlete a physical and psychological edge, removing minor restrictions and creating a body that is warm and ready to perform. Whether working with weekend warriors or elite competitors, the principles remain: prepare the tissue, alert the mind, and facilitate the training goals. By mastering these techniques, you elevate yourself from a therapist to a crucial member of the performance team.
Clinical Perspectives on Post Event Sports Massage Benefits
The conclusion of a competitive event marks a critical physiological shift. The athlete has pushed their metabolic and structural systems to the limit, creating an internal environment defined by oxidative stress, micro-trauma, and sympathetic nervous system dominance. In RSM's Sports Massage Course, we emphasize that the recovery phase is an active, vital component of the athletic cycle. When we analyze post event sports massage benefits, we are looking at a targeted intervention designed to transition the body from high-output stress to structural repair.
This transition is rarely instantaneous. While the body possesses innate healing mechanisms, professional intervention expedites the return to homeostasis. My experience in sports medicine confirms that the difference between prolonged fatigue and a rapid return to training often depends on the quality of care received in the hours immediately following the event.
The Physiology of Recovery
To effectively apply sports massage in a post-competition setting, we must understand the biological reality of the athlete. During the race or match, blood flow is diverted to skeletal muscles, and cortisol levels surge to mobilize energy. Once the activity ceases, the body must reverse these processes.
Massage applied in the immediate window – often called the “Golden Hour” – serves as a neurological catalyst. Our primary goal is not to fix specific injuries but to facilitate a parasympathetic shift. By applying rhythmic, broad-contact pressure, we stimulate mechanoreceptors that signal the central nervous system to lower heart rate and reduce muscle tone. If the athlete remains in a high-stress sympathetic state, their body prioritizes vigilance over repair.
Circulatory Dynamics
Historically, the industry claimed massage “flushed lactic acid.” Science has since clarified that lactate clears naturally during active cooldowns. However, the circulatory benefits of massage remain clinically significant. Post-activity muscles are often congested with interstitial fluid. This congestion increases internal pressure, impeding venous return and lymphatic drainage.
Through specific therapy applications, we mechanically assist the venous pump. We encourage the movement of stagnant fluid out of tissue spaces and into the circulatory system for filtration. This reduction in local edema lowers pressure on nociceptors (pain receptors), providing immediate relief and setting the stage for post-event recovery.
Restoring Athletic Performance and Managing DOMS
Recovery acts as the bridge to future athletic performance. An athlete who recovers slowly misses training sessions or trains with compromised biomechanics, which inevitably leads to overuse injuries.
After a grueling event, muscles often remain in a shortened, semi-contracted state. This heightened resting tone alters joint mechanics. For example, tight muscles in the hamstring group can posteriorly tilt the pelvis, changing the athlete’s gait and loading the lumbar spine incorrectly. By gently coaxing muscle fibers back to their resting length, we restore the optimal length-tension relationship. This ensures that when the athlete resumes exercise, their movement patterns are efficient and safe.
Addressing Muscle Soreness
One of the primary reasons athletes seek care is to mitigate Delayed Onset Muscle Soreness (DOMS). This soreness results from inflammation caused by connective tissue micro-trauma. While massage cannot undo the damage done during the race, it modulates the inflammatory cascade. Research suggests that massage reduces the production of inflammatory cytokines. By managing this inflammation, we reduce the severity of soreness, allowing the athlete to maintain mobility rather than locking up in stiffness patterns.
Specific Techniques and Safety in Event Massage
The protocol for event massage is distinct from maintenance or clinical work. The tissue is fragile and likely contains exercise-induced muscle damage (EIMD). Therefore, deep tissue work or aggressive trigger point therapy is contraindicated. Digging into compromised tissue will only exacerbate inflammation.
We train therapists to use fluid, continuous strokes. The application should be broad and compressive, maximizing surface area contact to move fluid without shearing fibers.
Key Techniques Include:
- Effleurage: Long, gliding strokes following venous return to move lymph fluid.
- Compressive Petrissage: Rhythmic kneading that pumps the muscle belly without aggressive pinching.
- Passive Stretching: Gentle mobilization to reset proprioceptors and restore range of motion.
- Vibration: Fine shaking movements to loosen muscle bellies without invasive pressure.
Contraindications
Safety is paramount. The post-competition body is vulnerable, and certain conditions require medical intervention rather than massage. Therapists must be vigilant for:
- Heat Stroke: Nausea, dizziness, cessation of sweating, or cold skin requires immediate cooling and medical aid. Massage can dangerously lower blood pressure in these cases.
- Acute Injury: Visible swelling or inability to bear weight suggests sprains or fractures.
- Hypothermia: In cold events, exposing skin can worsen a drop in core temperature.
The Lymphatic Role in Repair
A critical aspect of recovery is the lymphatic system, which relies on muscle contraction and movement to circulate fluid. After extreme exertion, interstitial spaces fill with metabolic debris. If the athlete remains sedentary after the finish line, this fluid stagnates.
Manual therapy acts as an external pump. By applying light, directional pressure, we advance this fluid into the lymph nodes for processing. This is particularly vital for ligament and tendon health, as these structures have poor natural circulation and rely on efficient fluid turnover for nutrient delivery.
Integrating Massage Therapy into the Training Cycle
An isolated session is beneficial, but consistent massage therapy yields the superior results. We encourage athletes to view treatments not as a luxury reward, but as a critical logistic of their training, equal to nutrition or sleep.
When an athlete incorporates regular structural checks, they establish a physiological baseline. The therapist learns their unique patterns of tension, allowing for faster problem-solving when anomalies arise. For the professional therapist, this means moving beyond a routine sequence and developing a strategy based on the specific movement demands of the sport. While the immediate post competition approach is generalized to address systemic fatigue, long-term care requires specific knowledge of the athlete’s biomechanics.
The Human Element in Sports Recovery
As sports science evolves, we see a surge in holistic recovery modalities. Technologies like pneumatic compression boots and cryotherapy are valuable, yet they lack the palpation skills of a human therapist. A machine cannot feel a localized area of hypertonicity or adjust pressure based on the athlete’s involuntary guarding response.
The human element in wellness remains irreplaceable. The ability to sense tissue quality – to detect the difference between a muscle that is simply tight and one that is nearing a cramp – is a skill honed through years of practice. At RSM, we teach that high-quality palpation is the primary diagnostic tool in sports recovery.
Dispelling the “No Pain, No Gain” Myth
One of the most persistent misconceptions we fight is the idea that effective treatment must hurt. especially in a post-event context, pain is counterproductive. It triggers a withdrawal reflex and sympathetic activation – the exact opposite of the relaxation response we are trying to engineer.
If a therapist digs an elbow into a fatigued, micro-torn hamstring, the body perceives it as a threat. We must educate both the athlete and the student that depth is not synonymous with effectiveness. Accessing deeper layers of tissue is achieved through patience and melting through superficial layers, not by forcing through them. In the recovery phase, less is often more.
Final Thoughts on Care
The protocol for recovery is complex because every body reacts to stress differently. Variables such as hydration, training volume, genetics, and environmental conditions all dictate the body’s response to exertion. Our job as specialists is to meet the athlete where they are, assessing their physical and mental state to apply the appropriate intervention.
When we maximize the recovery window through post-event sports massage, we do more than just reduce soreness. We facilitate the structural repair necessary for the athlete to continue doing what they love. By respecting the tissue, facilitating fluid flow, and calming the central nervous system, we elevate massage from a simple service to a crucial medical adjunct in the world of high-performance sports.
Navigating Contraindications for Deep Tissue Therapy
At RSM International Academy, we approach bodywork through the lens of sports medicine. This means viewing the body not simply as a structure to be manipulated, but as a dynamic biological system where every mechanical input creates a physiological cascade. In our Deep Tissue Massage Training, we emphasize that the most critical skill a therapist possesses is not the strength of their hands, but the discernment to know when not to treat.
Safety is the absolute foundation of our practice. My own background in sports medicine has instilled a deep respect for pathology. We must recognize that the profound changes induced by deep tissue massage – such as increased venous return, fascial manipulation, and autonomic stimulation – can become detrimental if the system is already compromised. Assessing these risks requires a sophisticated understanding of hemodynamics and inflammation. It is insufficient to merely memorize a list of conditions; you must understand the mechanism of risk to make informed clinical decisions.
Recognizing Systemic Contraindications
When a client presents with a systemic condition, the risk affects the entire body, not just a localized area. These are often absolute barriers to treatment. Deep tissue work places a significant demand on the circulatory and lymphatic systems. If the organs responsible for filtering and pumping fluids – specifically the heart, kidneys, and liver – are compromised, the sudden surge in fluid volume caused by massage can precipitate organ failure.
Hemodynamics and Vascular Risks
The movement of blood is central to the efficacy of our work, yet it also presents our most severe risks. In a sports medicine context, Deep Vein Thrombosis (DVT) is a critical pathology. A thrombus forms in the deep veins, usually in the leg. The heavy mechanical pressure of tissue massage can dislodge this clot, transforming it into an embolus that may travel to the lungs or brain with fatal consequences.
If you observe heat, redness, swelling, or a deep ache in a client’s calf, this is a medical emergency. We never massage a limb with suspected DVT. Similarly, uncontrolled hypertension poses a significant barrier. Vigorous bodywork can fluctuate blood pressure, creating unnecessary stress on arterial walls in clients with unstable cardiovascular systems.
Infection and Fever
We frequently encounter the misconception that one can “sweat out” a fever through massage. This is a physiological error. A fever indicates the body is fighting a systemic infection. By mechanically increasing circulation, we risk spreading the pathogen more rapidly. Furthermore, the metabolic demand of receiving therapy competes with the energy reserves the immune system requires to combat the infection.
Relative Contraindications and Adaptive Strategies
While some conditions require a full stop, relative contraindications require the nuanced judgment of a clinician. In these scenarios, therapy is possible, but treatment modifications are essential to ensure safety.
Acute Muscle Injury and Inflammation
We often see athletes immediately following an injury. There is a persistent myth that aggressive rubbing helps acute strains. In reality, applying deep pressure to acutely injured muscle or ligament tissue exacerbates the inflammatory response. During the acute phase (typically the first 72 hours), the body is stabilizing the area. Disrupting this process with heavy friction increases bleeding and delays healing.
However, this does not mean the client cannot be treated. We can work proximal or distal to the injury to manage compensatory tension and improve lymphatic drainage, provided we strictly avoid the site of acute trauma.
Oncology Considerations
Modern science has evolved our understanding of cancer care. We no longer view cancer as an absolute barrier due to fear of metastasis through circulation – simple exercise increases circulation more than massage does. The concern with oncology clients is fragility. Chemotherapy and radiation can compromise bone density and skin integrity. While aggressive deep tissue techniques are contraindicated due to the risk of bruising or fracture, gentle, modified massage therapy is often encouraged for pain management and anxiety reduction.
A Critical Massage Precaution
Certain physiological states require a complete shift in our approach. These are not always pathological, but they alter how the body responds to pressure and pain.
Pregnancy Massage Safety
Pregnancy massage is a distinct modality requiring specialized knowledge. The physiological changes during pregnancy include blood volume expansion, ligament laxity, and compression of the vena cava. Deep abdominal work is strictly contraindicated.
During the first trimester, many practitioners exercise extreme caution to avoid any correlation with spontaneous miscarriage. In later stages, positioning is critical to prevent supine hypotensive syndrome; side-lying positions are mandatory to ensure safety for both mother and fetus.
Pharmaceutical Interactions
A professional intake must always review the medications a client is taking. Drugs often mask symptoms or alter physiological responses.
- Analgesics: Painkillers alter pain perception. Since pain is our primary feedback loop during deep work, a client on heavy analgesics may not feel tissue damage occurring.
- Anticoagulants: Clients on blood thinners have reduced clotting ability. The micro-trauma associated with deep friction can cause extensive internal bleeding. In these cases, lightening the pressure is a mandatory massage precaution.
Assessing High-Risk Tissue
Beyond systemic issues, we must evaluate the structural integrity of the local area. If the tissue cannot support the mechanical load of compression, the therapy must be diverted.
The Spine and Skeletal Integrity
Osteoporosis affects bone density, making the spine and ribs particularly vulnerable. Deep compressive strokes or aggressive mobilization can easily fracture a rib in a client with advanced osteoporosis. This condition is often silent until a fracture occurs, so we must assess risk factors like age and history.
Similarly, recent fractures are a local exclusion. The vibration and shear forces of massage disrupt the callus formation necessary for bone union. While we can treat surrounding areas to alleviate cast-sickness, the fracture site itself demands stability.
Skin and Varicose Veins
Any breach in skin integrity – bacterial infections, open wounds, or burns – is a local contraindication. We must also be vigilant regarding varicose veins. These distended vessels have damaged valves and weakened walls. Direct pressure can cause the vein to rupture or dislodge a clot. We never apply stripping strokes over varicose veins; we work strictly around them.
The Professional Standard
Understanding these risks distinguishes a hobbyist from a professional. At RSM, we teach that confidence grows from knowing when to stop. We have a responsibility to act as a checkpoint in our client’s healthcare journey. By recognizing the signs of kidney dysfunction, identifying the symptoms of a blood clot, or respecting the complexity of a medical diagnosis, we protect our clients from harm.
If you encounter a condition that falls outside your scope, the correct course of action is referral. Requesting clearance from a physician is a mark of professionalism. It demonstrates that you prioritize safety above revenue. When we navigate contraindications with expertise, we ensure that massage remains a safe, effective tool for healing.
How Myofascial Release Works: A Sports Medicine Perspective
The Architecture of Human Connectivity
To truly understand the mechanism of effective manual therapy, we must look beyond isolated muscles and examine the environment in which they operate. For years, anatomy instruction treated the white, fibrous tissue surrounding muscles as mere packaging. We now know that this tissue, the fascia, is the continuous, integrated web that holds the human body together.
Fascia consists of elastin, collagen, and a viscous fluid called ground substance. It surrounds every muscle, nerve, and organ. When this system is in good health, the fascial layers glide frictionlessly, allowing for uninhibited mobility. However, trauma, inflammation, or poor posture can alter the chemical composition of the ground substance. The fluid becomes gelatinous, leading to the formation of fascial restrictions.
These restrictions glue layers of tissue together, creating drag on the biomechanical system. This tension is often transmitted to distant areas; a restriction in the hip can eventually manifest as pain in the back. This interconnectedness explains why treating only the site of symptoms often fails. To provide lasting relief, we must address the tensile stress in the connective tissue matrix.
The Mechanics of Myofascial Release
The physiological basis of this therapy relies on specific properties of connective tissue: piezoelectricity and thixotropy. When a therapist applies sustained pressure to restricted tissue, these two responses are triggered.
Piezoelectricity is the electric charge generated in solid materials, like collagen, under mechanical stress. This bio-electric response stimulates fibroblasts to reorient the collagen fibers in a functional alignment. Simultaneously, thixotropy occurs. The ground substance is thixotropic, meaning it becomes less viscous when stressed or agitated. Under the heat and pressure of manual manipulation, the ground substance shifts from a gel-like state to a fluid sol-state. This reduces friction and allows the collagen fibers to slide apart.
In RSM’s Dynamic Myofascial Release Course, we emphasize that myofascial release is not a contest of force. If pressure is too aggressive, the body triggers a stretch reflex, causing muscles to guard the area. True release requires engaging the tissue barrier with just enough tension to initiate changes without provoking a defensive reaction.
Addressing Muscle Tension and the Trigger Point
While fascial restrictions affect the gliding potential of tissue, we must also address muscle tension within the fibers themselves. Chronic stress often leads to the development of a trigger point – a localized area where sarcomeres are locked in permanent contraction.
A trigger point chokes off local blood supply, causing a metabolic crisis that sensitizes pain receptors. Treating myofascial trigger points requires ischemic compression. We apply direct pressure to occlude blood flow temporarily; when released, fresh blood flushes the tissue, washing away metabolic waste and breaking the pain-spasm cycle.
This distinction is vital for any healthcare provider. A patient may present with pain, but the source could be a referral pattern from a distant trigger point. Understanding whether the issue is a fascial adhesion or a contractile knot is the key to effective treatment.
Neurological Implications and Release Techniques
The mechanical changes in the tissue are only half the equation. The fascia is densely innervated with mechanoreceptors. When we apply slow, deep shear forces, we communicate directly with the autonomic nervous system, lowering sympathetic tone (fight or flight) and shifting the patient toward parasympathetic dominance (rest and digest).
Myofascial pain syndrome is often perpetuated by a sensitized nervous system. By providing non-threatening sensory input, myofascial release therapy is able to down-regulate the perception of threat, allowing the brain to learn to move the body without anticipating pain.
In clinical practice, we utilize various release techniques:
- Direct Release: Sinking into the tissue and dragging across the restriction to lengthen matted fibers.
- Active Release: Having the patient move a joint through its range while the therapist pins the tissue, restoring flexibility.
There is often confusion regarding self-myofascial release, such as foam rolling. While these tools can hydrate tissue and provide temporary pain relief, they lack the specificity of a skilled therapist. A foam roller cannot detect the subtle shift in texture that indicates a release. However, they remain valuable for maintaining fascial tissues between sessions.
Integrating Therapy into Sports Medicine
The back is a prime example of where fascial failure converges. The thoracolumbar fascia acts as a hub for force transmission. Research supports the view that stiffness in this large fascial sheet, rather than disc pathology, is a primary driver of non-specific lower back pain. By restoring the sliding potential of the thoracolumbar fascia, we reduce the compressive load on the spine.
In sports medicine, we view physical therapy as a means to improve efficiency. A restricted fascial system absorbs energy. By clearing adhesions, we reduce the internal friction of the athlete, allowing them to move freely and recover faster.
Ultimately, the goal is to restore function and self-regulation. Myofascial release transforms the practitioner from a technician into a clinician who interprets the unique physiological puzzle of the body. By respecting the intelligence of the fascial system, we unlock a potential for healing that goes far beyond simple relaxation.
Identifying Common Mistakes in Massage Practice
Many practitioners enter the field of bodywork with strong hands and good intentions, yet they often find their clinical results plateauing. At RSM International Academy in Chiang Mai, students from around the globe come to learn the precision of sports medicine. As they practice, I frequently observe a distinct set of errors that can prevent therapists from achieving mastery.
True expertise in bodywork is not merely about learning a sequence of strokes; it is about understanding the physiological narrative of the human body. While teaching RSM’s Deep Tissue Massage Course, for example, I emphasize the logic behind the touch. The difference between a mediocre session and a transformative treatment often lies in avoiding fundamental errors in judgment. These errors rarely stem from a lack of effort but from a lack of anatomical understanding or a failure to interpret the body’s cues correctly.
Refining one’s craft requires an honest audit of current habits. By identifying the technical and procedural gaps in our work, we elevate the entire profession. Here, we analyze the specific areas where practitioners often falter and how sports medicine principles provide the solution.
Overlooking the Client Intake and History
The most critical error in massage therapy often occurs before the client even lies on the table. In the rush to begin manual work, many therapists skip the assessment phase. This is a fundamental failure in clinical logic; you cannot treat what you do not understand. In a spa setting, a cursory glance at a form might suffice, but in a medical or sports context, the client intake is the blueprint for the entire treatment.
I teach my students that the history of an injury dictates the protocol. If a client presents with lower back pain, a generic rubdown is insufficient. We must know the mechanism of injury. Was it acute? Is it chronic? Without this data, the therapist works blindly, hoping to stumble upon relief rather than engineering it.
We must also verify contraindications. Conditions involving the skin, circulatory system, or acute inflammation change the rules of engagement. Furthermore, the intake establishes a baseline. Without understanding the client’s range of motion or pain levels before we start, we have no metric to judge the success of the sessions.
Prioritizing Routine Over Specific Massage Therapy Needs
There is a seduction in the familiar. Novice massage therapists often cling to a set routine because it feels safe. They learn a sequence in school and apply it indiscriminately to every body they encounter. This approach is the antithesis of effective massage therapy.
Every body presents a unique topography of tension and dysfunction. When a therapist operates on autopilot, they miss the specific needs of the tissue in front of them. In sports medicine, we treat the dysfunction, not the routine. If a client has a rotator cuff limitation, spending time on their calves simply to “complete the full body routine” is a misuse of time.
Effective massage therapy requires adaptation. The plan you form at the start of the session must be fluid. If I encounter rigid fascia in the thoracic spine, I must alter my strategy to address it. Sticking to a script when the body is asking for something different is a sign of inexperience. We must be willing to discard the routine in favor of clinical necessity.
Ignoring Client Cues and Pain Thresholds
A pervasive myth in the industry is that pain equals progress, but this is anatomically incorrect. While some discomfort is natural when addressing adhesions, ignoring client pain signals triggers the sympathetic nervous system. When the body perceives a threat, the muscles guard against the intrusion, making deep work impossible.
If a client is holding their breath, clenching their fists, or flinching, the pressure is too high. The therapeutic window exists on the edge of “good pain,” where the nervous system remains calm enough to allow the release. If we override these signals in pursuit of a knot, we cause micro-trauma, resulting in post-treatment soreness that exceeds the therapeutic benefit.
The experience of the client must remain the compass. We must distinguish between the sensation of release and the sensation of damage. Listening to the body involves feeling the tissue push back. When the muscle pushes back, we must soften, not harden.
Misunderstanding the Role of Client Comfort
In a clinical environment, elements like temperature or bolster placement are not “spa fluff.” They are physiological necessities. Client comfort is essential for recovery because we are manipulating the nervous system as much as the musculoskeletal system. If a client is cold, their muscles contract. If their neck is strained due to poor face-cradle adjustment, the cervical extensors cannot relax.
The equipment we use plays a massive role here. The table must support the body neutrally. If a client is lying prone and their lower back is compressed, no amount of lumbar work will resolve their pain because the position itself is the aggravator. Relaxation is not just for wellness spas; it is the state in which healing occurs. If the client is physically uncomfortable, their body remains in a state of low-level stress, negating much of our work.
Technical Mistakes and Lack of Feedback
Beyond conceptual errors, there are physical common mistakes in how massage is applied. The most frequent is using small muscle groups—hands and wrists—rather than leveraging core body weight. This leads to erratic pressure and therapist burnout. Another error is working too fast. Fascia needs time to change state; quick, jagged movements trigger the stretch reflex. To access deep layers of muscle, we must sink in slowly.
Crucially, the session does not end when the manual work stops. A vital component of growth is integrating client feedback. We need to ask specific questions regarding range of motion and pain levels. “How does that shoulder rotation feel now compared to when you walked in?”
We must also document this. Session notes are the scientific record of our practice. Failing to keep detailed notes means we start from zero every time the client returns. In a medical context, we need to track the trajectory of recovery to see if our techniques provided lasting relief.
The Professional Gap and Education
There is a distinct line between a hobbyist and a professional. One of the massage mistakes I often see is the blurring of boundaries. The therapy room is a vulnerable space, and the focus must remain entirely on the client. The therapist’s energy must be grounded and neutral.
We must also view the experience as an educational partnership. A common failure is neglecting to provide aftercare advice. If we release a tight hip flexor but the client returns to the same bad habits, the issue will return. We must explain the “why” behind the “what.” When a client understands the source of their pain, they become compliant partners in their recovery.
Becoming a True Clinician
Correcting these errors requires humility and a dedication to continuous learning. The field of sports medicine is always evolving, and our practice must evolve with it.
By prioritizing the client intake, respecting physiological limits, ensuring client comfort, and refining our technical execution, we move beyond being mere service providers. We become true clinicians. At RSM International Academy, this is the standard we set. The difference between a good massage and a great one is often just the removal of these mistakes. When we stop rushing and start truly listening to the tissue, the results speak for themselves.
Understanding the Real Benefits of Hands-On Massage Workshops
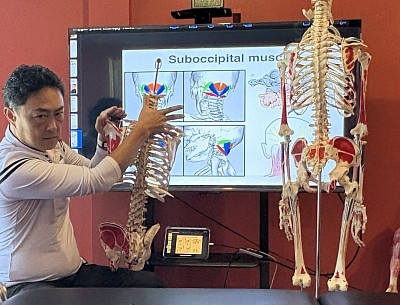
At RSM International Academy, we operate on the belief that while theory is essential knowledge, tactile practice makes it useful. RSM’s massage workshops in Thailand bridge the gap between academic sports medicine and the intuitive flow of massage. I have often seen profound growth in a therapist happen during the struggles and subsequent breakthroughs that can occur in the course of a massage workshop.
The Necessity of Practical Application
Anatomy is three-dimensional and dynamic. A student may memorize where the piriformis sits, but locating it on a rigid model is vastly different from palpating it on a professional athlete. Practical application is the only method that teaches the fingers to “see” beneath the skin.
In a live classroom, we encounter the reality of bio-individuality. When we guide students through hands-on learning, we teach them to navigate varying tissue densities in real-time. This is where the development of tactile sensitivity begins. It is the process of calibrating pressure not to an arbitrary standard, but to the specific feedback of the tissue. In our sessions, instructors physically adjust a student’s hand placement, ensuring they understand the physical sensation of a correct technique.
How Training Helps Students Build Muscle Memory
Massage is a kinetic profession requiring the therapist to use their entire body to generate force. Training helps students build muscle memory, allowing the mechanics of the treatment to become second nature. When the body moves efficiently, the mind is free to focus on the client’s response.
Through rigorous hands-on repetition, the movements of massage therapy shift from conscious effort to automatic movement. This conditioning also serves a protective function. Learning massage techniques can boost your personal well-being by instilling ergonomic habits that prevent burnout. In a workshop, we prioritize longevity, teaching students to generate pressure from their core, a distinction that adds decades to a massage practice.
Refining Complex Massage Techniques
There is a significant difference between rubbing skin and engaging deep fascia. Mastering this distinction requires guidance. Take deep tissue massage, for example. A common misconception is that deep tissue equates to heavy force. In reality, it refers to the specificity of the target tissue massage.
In our courses, we dismantle these techniques. We explore how to sink through superficial layers without triggering a guarding response. This nuance is impossible to acquire in isolation. It requires an instructor to place their hand over the student’s hand, allowing them to feel the precise moment the tissue releases. Exploring these boundaries in a supervised environment allows students to understand the limits of range of motion without risking injury.
How Experience Allows Therapists to Trust Their Instincts
Data and intuition are partners in clinical practice. Intuition is simply immediate pattern recognition based on accumulated experience. Experience allows therapists to recognize subtle cues – a change in breathing or a muscle flinch – and adjust their approach instantly.
We encourage students to trust their instincts, but only after those instincts have been honed by feedback. A massage workshop provides a safety net where students can test their intuitive hits. If they feel drawn to work on the hip flexors for a client with back pain, they can verify the anatomical logic with an instructor. This fosters a confidence that is a direct result of hands-on experience.
The Role of Continuing Education for Professional Growth
The field of sports medicine is evolving. Continuing education is the vessel through which a therapist stays relevant. Workshops offer a unique environment for professional growth because they are collaborative. Students learn by trading treatments, receiving therapy while giving it. Being on the receiving end clarifies a technique’s effect in a way that delivering it never can.
Furthermore, teaching workshops or participating in them creates community. Gathering with peers to refine massage skills reinvigorates passion. At RSM, practitioners attend our school to refine the quality of their touch and reconnect with their vocation.
Elevating Your Massage Practice
Ultimately, the goal of training is to improve outcomes for clients. Patients require a therapist who can assess and treat with accuracy. Workshops that focus on assessment skills bridge the gap between a spa treatment and clinical therapy.
When a therapist can explain the “why” behind a treatment and demonstrate results through practical manual therapy, they build trust. Problem-solving is a skill best sharpened through direct mentorship and practice.
Why We Emphasize Hands-On Learning
At RSM International Academy, our approach is rigorously grounded in modern sports medicine. We believe that hands-on training is the only way to honor the complexity of the human form. Students discover that their body is their primary tool, and it must be used with skill to be effective.
The benefits of this approach are clear:
- Safety: Supervision ensures techniques do not risk injury.
- Efficacy: Feedback ensures pressure creates physiological change.
- Adaptability: Students learn to modify techniques for different body types.
- Confidence: Repetition builds neurological pathways for assured movement.
To master this craft, one must engage with it physically. We invite you to join us and elevate your understanding of the human body from the academic to the palpable. This is the path to true mastery in massage.
Assessing Progress in Massage Therapy
At RSM International Academy, one way in which we differentiate between a relaxation technician and a sports medicine professional is in their ability to measure change. In the realm of advanced bodywork, intention is insufficient without verification. When designing the curriculum of RSM’s Trigger Point Therapy Course and other foundational modules, my objective was to elevate the standard of manual medicine by integrating rigorous scientific methodology with established techniques. A vital component of this integration is the systemic analysis of outcomes.
Without a robust framework for tracking improvement, a practitioner is merely guessing. We navigate a complex landscape of musculoskeletal pathology, and to do so, we must rely on data rather than intuition alone. Understanding the trajectory of an individual requires us to move beyond simple questions of comfort and into the realm of critical clinical reasoning.
The Role of Evaluation in Therapeutic Practice
The foundation of any successful intervention lies in the initial intake and the continuous monitoring of variables. In sports medicine, we do not simply apply friction or compression; we apply a specific stimulus to achieve a specific physiological response. To know if that response has occurred, we must have a baseline.
If we fail to establish a baseline, we cannot claim that our work has efficacy. We might observe that an individual feels better, but “feeling better” is subjective and fleeting. Clinical success is defined by reproducible, functional improvement. This requires a shift in mindset. We must view every session not as an isolated event, but as a data point in a longer timeline of care.
We teach our students that the treatment room is a laboratory. The variables are the manual techniques we apply, and the results must be observable. By establishing clear metrics at the onset, we protect both the practitioner and the recipient. The practitioner is protected from stagnation, while the recipient is protected from ineffective care.
Moving Beyond Intuition: The Massage Therapist as Analyst
There is a pervasive myth in our industry that “good hands” are all that is required to heal. While manual dexterity and sensitivity are prerequisites, they are not the entirety of the discipline. A competent massage therapist must also be a skilled analyst. The tactile information we receive through our fingertips is only one part of the diagnostic puzzle.
When we rely solely on what we feel in the tissue, we are subject to confirmation bias. We might believe a muscle feels “looser,” but does this translate to increased range of motion or decreased discomfort during activity? Not always. Therefore, we must validate our palpation findings with external, objective markers.
This transition from an intuition-based model to an evidence-based model is what separates recreational bodywork from massage therapy. It demands that we adopt the rigor of physical therapists and orthopedists. We must become comfortable with the language of pathology and the tools of measurement.
Establishing the Baseline
The initial consultation is where the trajectory of care is set. Before a hand is laid on the body, we must gather information through detailed history taking. We look for red flags, contraindications, and the mechanism of injury.
However, the history is only the narrative; the physical evaluation is the fact-checking. At RSM, we emphasize the importance of distinct, reproducible tests. If an individual presents with shoulder issues, we measure active and passive range of motion. We identify the specific arc of limitation. This initial data collection creates the baseline against which all future success is measured. It is impossible to claim that a condition has improved if we did not quantify the condition’s severity at the start.
The Anatomy of a Functional Goal
One of the most significant errors in massage therapy is setting goals that are too vague. A goal like “fix back issue” is immeasurable. To objectively track progress, we must convert these vague desires into concrete functional goals.
We utilize the SMART criteria but adapt it for the context of manual therapy. A functional goal focuses on activity. Instead of “reduce knee discomfort,” we aim for “increase knee flexion to 120 degrees to allow squatting without compensation.”
By anchoring the outcome to a specific physical action, we align our treatment with the patient’s daily life. This shifts the focus away from the sensation of discomfort, which can be volatile, and towards capacity. If they can perform a task today that they could not do yesterday, the therapy is working.
Visual Assessment and Postural Analysis
Before we touch, we look. Visual assessment provides the first layer of objective data. We observe the individual standing, walking, and moving through basic patterns. The human body is an architectural structure; deviations in the foundation will inevitably cause cracks in the walls.
We look for landmarks. Are the shoulders level? Is there an excessive anterior pelvic tilt? These are clues to the underlying soft tissue puzzle. In a massage therapy treatment context, we often use grid photography. Taking a photo of the patient against a postural grid during the first session provides an undeniable record of their starting point. Repeating this after several sessions provides visual proof of the benefits of the work.
We also analyze gait. A shortened stride or a lack of arm swing points to specific muscular inhibitors. We document these observations in the soap note to ensure they are revisited in future sessions.
Palpation Assessment: Reading the Tissue
While palpation assessment is subjective, it can be systematized to increase reliability. We are assessing specific qualities of the tissue: texture, temperature, tenderness, and tone.
- Texture: We look for fibrosis, adhesions, and scar tissue.
- Temperature: Heat indicates acute inflammation; coolness suggests ischemia.
- Tone: We assess resting muscle tension.
We map trigger points and note their referral patterns. By documenting findings precisely – such as a trigger point in the upper trapezius referring sensation to the temple – we can track if the referral pattern recedes or centralizes over time. This centralization is a key indicator of improvement in massage therapy.
Range of Motion (ROM): The Gonio is Your Friend
Goniometry is an essential skill for any serious massage therapist. Measuring the degrees of flexion or rotation provides a hard number. If an athlete has 45 degrees of cervical rotation during intake and 60 degrees after three sessions, we have proof of mechanical improvement.
We distinguish between Active Range of Motion (AROM) and Passive Range of Motion (PROM). AROM assesses the willingness to move and contractile ability, while PROM assesses the joint capsule and inert tissues. Discrepancies between the two provide immediate direction for the treatment. If AROM is limited but PROM is normal, the issue is likely muscular weakness or neurological inhibition, requiring a different strategy than a joint restriction.
Orthopedic Testing in Massage
To refine our understanding of the client condition, we employ orthopedic special tests. These maneuvers stress specific structures to reproduce symptoms. While diagnosis is the realm of the physician, functional differentiation is the realm of the therapist.
For example, discriminating between lumbar disc involvement and piriformis syndrome is crucial. Knowing this distinction changes the massage therapy treatment entirely. We would treat a disc issue with stabilization, whereas piriformis syndrome responds to specific compression. Tracking the results of these tests over time, and noting when a positive test becomes negative, is a primary method to objectively track progress.
Developing Dynamic Treatment Plans
The data collected during assessment is useless if it does not inform the strategy. A strategy is not a static document; it is a dynamic roadmap that evolves based on the individual’s response. At RSM, we teach that the treatment plans dictate the technique.
If the evaluation reveals a joint capsule restriction, the strategy must prioritize mobilization over deep tissue massage. The roadmap bridges the gap between the current state and the desired goal. It outlines the frequency of visits, the specific treatments, and the expected timeframe. Crucially, it sets benchmarks for re-evaluation. We do not treat indefinitely; we treat for a set period, then we measure.
Documentation and the SOAP Note
The mechanism for tracking this data is the SOAP note (Subjective, Objective, Assessment, Plan). Writing concise, accurate notes is a professional obligation.
- Subjective: What the individual reports.
- Objective: What the therapist observes and measures.
- Assessment: The professional opinion on what the data means.
- Plan: The strategy for the current and future sessions.
Consistent documentation allows us to identify patterns and correlations that would otherwise be lost. Furthermore, it is the primary tool for collaboration. If a patient is referred to a specialist, our notes provide a detailed history of the soft tissue therapy attempted. This elevates the perception of the therapist to a member of the allied health team.
Clinical Reasoning: The Intellectual Core
Data collection is mechanical; reasoning is intellectual. It is the process of synthesizing findings to form a hypothesis. This is where the expertise of the massage therapist shines. We must ask why the data looks the way it does.
If an individual presents with low back issues and tight hamstrings, reasoning prevents us from assuming the hamstrings are the sole cause. Are they tight to protect a hypermobile pelvis, or due to prolonged sitting? The treatment for these scenarios differs vastly. Assessing progress requires us to constantly challenge our hypotheses. If a person is not improving, we must use our reasoning skills to determine why and adjust the strategy.
The Feedback Loop: Micro and Macro Assessment
The cycle of care follows the pattern: Assess, Treat, Re-assess. Re-evaluation should happen within the session (micro-assessment) and at set intervals (macro-assessment).
Micro-assessment occurs immediately after a technique. If we perform a release to improve rotation, we check rotation immediately. Did it work? If yes, we proceed. If no, we adjust. This real-time feedback loop ensures no time is wasted on ineffective maneuvers during the massage.
Macro-assessment occurs every few sessions. We repeat the baseline tests. If the metrics show improvement, the therapy treatment is working. If stagnant, the strategy must change. Referring a patient out when progress stalls is a hallmark of professional integrity.
The Role of Research and Evidence-Based Assessment
We encourage our students to stay abreast of current research. The field of manual medicine is evolving. By integrating evidence-based assessment tools, we ensure our practice remains effective.
Research helps us understand the mechanisms behind progress, validating the physiological effects of massage therapy on symptom modulation and tissue elasticity. When we understand the science we can explain the “why” to our patients, improving compliance.
The Client’s Role and Psychological Impact
We must acknowledge that we are not the sole agents of change. The individual plays a pivotal role. Progress is often dictated by what they do when they are not on our table. Part of our evaluation involves tracking compliance with corrective exercises and lifestyle modifications.
There is also a profound psychological benefit to objective assessment. Patients often feel helpless in the face of chronic issues. When we show them data, for example a graph of improving range of motion, we restore their sense of agency. The massage therapist facilitates this by acting as a mirror, reflecting their progress back to them in undeniable facts.
Handling Regression and Plateaus
No recovery path is linear. A competent therapist anticipates regression. A flare-up of symptoms may simply be a reaction to increased activity as the person feels better. When a plateau occurs, we return to the assessment to look for missed variables or psychosocial stressors.
We use data to contextualize the plateau. Showing a patient that their range of motion has maintained gains, even if symptoms fluctuate, prevents discouragement and keeps the focus on the long-term trend.
Conclusion: The Precision of Care
At RSM International Academy, we believe the difference between a good therapist and a great one is the ability to navigate the complexity of the human body with precision. Assessment is the compass we use for this navigation.
By rigorously establishing baselines, utilizing objective metrics like visual assessment and goniometry, maintaining detailed soap notes, and engaging in continuous critical reasoning, we ensure every session has a purpose. We move beyond the vague hope of healing into the concrete realm of rehabilitation.
Ultimately, the goal is to render ourselves unnecessary. We assess progress to know when the individual has reached independence. When the dysfunction is resolved and the treatment plans are completed, we have succeeded. This success is not a feeling; it is a fact, proven by the data. This is the standard of care we advocate for, and it is the future of massage therapy.
Massage Therapy Ethics and Boundaries in Clinical Practice
True clinical excellence extends beyond anatomical knowledge or manual dexterity. At RSM International Academy, I often emphasize that without a foundation of trust, the physiological response to treatment diminishes. And so understanding massage therapy ethics is not merely a legal formality; it is a clinical necessity for effective treatment.
We operate in a space where physical touch is the primary modality, and this reality inherently creates vulnerability. Clients arrive in pain and place their physical well-being in our hands. The therapist holds a significant amount of power, and recognizing and respecting this power differential defines the professional. The standards required for modern practitioners, blending technical protocols with an ethical framework, are a key component of the Deep Tissue Massage Course and other courses we teach at our school in Chiang Mai.
Why We Maintain Professional Boundaries
The relationship between a clinician and a client is asymmetrical. The client seeks help, and the therapist provides it. Establishing clear professional boundaries is essential to protect the client from exploitation and the therapist from liability. When boundaries blur, the therapeutic objective becomes clouded.
Boundaries function as the parameters that define the edge of appropriate behavior. Physically, they dictate how we touch and drape a client. Emotionally, they prevent the therapist from offloading personal burdens onto the patient. Intellectually, they keep the conversation focused on the treatment plan rather than personal opinions.
Many new therapists struggle with the emotional component. We enter this field to help people, yet empathy without boundaries leads to burnout. If a therapist becomes too emotionally invested in a client’s outcome, they lose the objectivity required to make sound clinical decisions.
From a sports medicine perspective, boundaries directly influence the autonomic nervous system. A client who feels unsure about the therapist’s intentions remains in a state of sympathetic arousal. Muscle tonus increases. Conversely, when a client perceives a safe environment, they shift into parasympathetic dominance. Poor boundaries are limiting your potential to achieve these physiological results.
The Role of Informed Consent
Trust is legally and ethically operationalized through informed consent. This is not a passive signature on an intake form. It is an active, ongoing dialogue between the therapist and the client. The client must understand what will happen to their body and the potential risks involved.
If a practice involves working near sensitive areas, such as the adductors or the pectorals, the therapist must explain the clinical relevance before making contact. Informed consent includes the scope of treatment, rationale, risks, and the explicit right to refuse.
At RSM, we teach that consent is dynamic. It can be withdrawn in the middle of a session. If a client tenses up or verbalizes discomfort, the therapist must stop immediately. Ignoring non-verbal cues is a violation of the therapeutic relationship.
Navigating Dual Relationships
A specific challenge in the wellness industry is the occurrence of dual relationships. This happens when a therapist and a client share a role outside of the clinical setting. They might be members of the same gym or belong to the same social circle. In smaller communities, these overlaps are often unavoidable.
While not all dual relationships are unethical, they are high-risk. The danger lies in the confusion of roles. If a therapist treats a close friend, the casual nature of the friendship may erode the professional structure of the session. The client might expect a discount, or the therapist might share personal problems during the massage. This dilutes the clinical focus.
To manage this, professionals must compartmentalize. When the session begins, the friendship is suspended, and the clinical protocol takes over. We recommend avoiding treatment of close family members or romantic partners whenever possible. If a dual relationship cannot be avoided, the therapist must discuss the potential conflicts with the client to ensure the professional dynamic remains intact.
Sexual Conduct and Zero Tolerance
There is no gray area regarding sexual conduct in a healthcare setting. Any sexual activity or romantic pursuit within the therapeutic relationship is a violation of ethical standards. The power differential renders the client unable to give valid consent to sexual activity with their therapist.
Sexual misconduct includes inappropriate draping, sexualized comments, or touching clients with sexual intent. At RSM, we instill a zero-tolerance mindset. The safety of the client is paramount. Even the appearance of impropriety can destroy a career.
If a client initiates sexual behavior, massage therapists must end the session immediately, leave the room, and document the incident. This strict separation protects the industry. Massage therapy has fought hard to shed historical stigmas and establish itself as a legitimate healthcare profession. We must uphold these standards to maintain our standing in the medical community.
Financial Boundaries and Ethical Practices
Ethics extend to the administrative side of a practice. Financial boundaries ensure clarity and prevent resentment. This includes setting clear fee structures and cancellation policies.
Transparency is key. Clients should never be surprised by the cost of a session. Hidden fees create distrust. If a therapist offers a sliding scale, these must be applied consistently to avoid accusations of discrimination.
Bartering services is a common trap. While it seems like a fair exchange, the value of services rarely aligns perfectly. If bartering is necessary, it should be formalized with a contract and treated as a taxable transaction to ensure ethical practices.
Handling Ethical Dilemmas
Textbooks cannot cover every scenario. Ethical dilemmas arise when two correct principles conflict or when the right course of action is unclear. Consider a scenario where a client offers a therapist an expensive gift. Accepting it might compromise professional distance, while rejecting it might damage rapport.
To navigate these moments, therapists should utilize an ethical decision-making model:
- Identify the Problem: Is this a legal, moral, or technical issue?
- Consult the Code: Refer to the code of ethics provided by your certifying body.
- Assess the Context: Does this serve the client’s best interest?
- Seek Supervision: Discuss the situation with a mentor.
Developing the capacity for ethical reasoning allows the practitioner to navigate complex human interactions without losing their professional footing.
Confidentiality and Ethical Conduct
What happens in the treatment room stays in the treatment room. Confidentiality is the bedrock of ethical conduct. Clients share medical histories and body insecurities during a session. This information is protected.
Therapists must secure client files physically and digitally. Discussing a client’s condition with a spouse or friend, even without using names, can lead to accidental breaches. In a tight sports community, anonymous details are often enough to identify a person.
Exceptions to confidentiality are specific: when the client gives written permission, or when there is an immediate threat of harm. Adhering to these privacy rules builds trust and ensures the safety of the patient.
Our Commitment to High-Quality Care
At RSM International Academy, we view ethics as the skeleton of our profession. Just as the skeletal system provides the structure for muscles to generate movement, ethical standards provide the structure for therapeutic techniques to generate healing.
We challenge our students to look inward. Maintaining professionalism is an internal discipline before it is an external behavior. It requires self-awareness and the humility to admit when a situation is beyond one’s capability.
Maintaining this level of integrity filters out chaos and drama from the clinical environment. This allows the work to take center stage. When the boundaries are solid, the client stops worrying about the environment and focuses entirely on the sensory input of the massage. This maximizes the healing response.
In the competitive field of sports medicine and bodywork, reputation is everything. A therapist might have “golden hands,” but if they push boundaries, their practice will fail. Maintaining professional integrity is a business strategy. High-profile athletes require a therapist who is reliable and discreet.
By adhering to these rigorous standards, we elevate the entire profession. We move massage therapy away from the fringes of relaxation and firmly into the realm of respected healthcare. By mastering the ethics of our trade, we honor the services we provide and the people who trust us with their care.
Ultimately, strong boundaries do not separate us from our clients; they allow us to connect with them safely. They create the distinct channel through which healing can occur. Without them, we are merely touching. With them, we are providing therapy.
Choosing a Sports Massage Specialization for Your Career
Why Massage Therapy Requires Focus
I founded RSM International Academy with a distinct mission: to elevate the standard of manual therapy education. The human musculoskeletal system is too complex for a generalized approach to be effective in treating chronic pain or injury. Consequently, massage therapy must be viewed as a discipline rooted in functional anatomy and biomechanics.
Many aspiring therapists fall into the trap of becoming generalists. Without a clear focus, a therapist often struggles to provide the targeted relief that clients with specific pathologies require. To truly succeed and make a tangible impact on a client’s health, one must choose a path. The decision to select a distinct area of expertise is the defining moment in a professional journey. At RSM, we believe that choosing to specialize is not optional; it is essential for clinical efficacy.
The Role of Sports Massage in Modern Health
The landscape of wellness is shifting. The demand for sports massage has expanded significantly, moving beyond the exclusive domain of elite competitors. Today, general populations suffering from postural deviations, “tech neck,” and repetitive strain injuries turn to sports specialists for solutions. This evolution has solidified sports massage as a fundamental component of modern health maintenance for everyone, not just athletes.
In the Sports Massage Course at RSM, students learn that sports massage is about understanding the kinetic chain. Pain in the lower back, for instance, is often a result of tightness in the hamstrings rather than a local issue. A therapist with general training might only treat the symptom. In contrast, a therapist with specialized training in sports modalities will assess the global mechanics of the body. This level of clinical reasoning distinguishes a true professional from a hobbyist.
How to Specialize in Clinical Rehabilitation
Once you recognize the baseline value of massage, the next logical step is to specialize in clinical rehabilitation. This sector requires a rigorous understanding of pathology. Clinical settings demand that massage therapists possess the ability to communicate effectively with medical professionals, such as physiotherapists and orthopedic surgeons.
Specifically, we differentiate between routine maintenance massage and Remedial Massage. Remedial work focuses on resolving specific dysfunctions, such as Frozen Shoulder or Sciatica. To succeed in this niche, one must master detailed palpation skills. You must be able to distinguish between hypertonic muscle tissue and fibrotic adhesions. This sensitivity is difficult to learn from a textbook; it requires extensive hands-on training under expert supervision. As a result, massage therapists who master these clinical skills become indispensable, often securing a more stable and lucrative career.
Defining Your Path in Sports Therapy
There is a distinct difference between sports massage and sports therapy. While sports massage often focuses on pre-event preparation and post-event recovery, sports therapy encompasses a broader spectrum of injury management. For students deciding on their future, it is vital to understand where your passion lies.
Therapeutic massage serves as the foundation for both, but the application differs. In a sports therapy context, you might integrate massage with Proprioceptive Neuromuscular Facilitation (PNF) stretching or corrective exercise protocols. My background in sports medicine influences how we teach these concepts. We emphasize that massage is a tool for correction. If a client suffers from medial tibial stress syndrome, a sports therapy approach involves releasing the deep posterior compartment while simultaneously addressing gait mechanics.
The Importance of Advanced Massage Techniques
To execute these treatments effectively, a therapist must command a repertoire of advanced massage techniques. Standard Swedish strokes are insufficient for breaking down scar tissue or releasing deep fascial restrictions. Therefore, we prioritize modalities like Deep Tissue Massage, Trigger Point Therapy, and Dynamic Myofascial Release.
Deep Tissue Massage, when taught correctly, is not about applying brute force. It is about sinking through superficial layers to access deeper musculature safely. Without precise anatomical knowledge, deep pressure can be harmful. This is why training at RSM includes rigorous study of functional anatomy. Uniquely, we offer students the opportunity to participate in Cadaver Clinical Palpation training in collaboration with the Faculty of Medicine at Chiang Mai University. Seeing the texture of muscles and fascia in a cadaver lab transforms abstract concepts into reality, allowing for a level of medical massage precision that is rare in the industry.
Advancing Your Career Through Training
Building a sustainable career in this industry requires a commitment to lifelong learning. The initial diploma is merely the entry ticket. At RSM, we limit our class sizes to a maximum of seven students to ensure individual attention. In a large massage school, bad habits can easily go unnoticed. In our intimate setting, we correct posture and technique immediately.
Furthermore, credibility is paramount. While a certification board sets the minimum standards, elite training exceeds them. Clients are becoming increasingly educated; they seek massage therapists who can explain the physiological “why” behind the treatment. When graduates can articulate how massage aids venous return or reduces cortisol, they build trust. This trust is the currency of a successful career.
RSM International’s Approach to Massage Education
- Evidence-Based Curriculum: Every technique is grounded in sports medicine principles, focusing on clinical reasoning rather than rote routines.
- Anatomical Precision: Our unique cadaver labs ensure students understand exactly what lies beneath their hands.
- Holistic Integration: We combine massage with posture correction and movement therapy.
- Mentorship: I personally oversee the development of our students, ensuring they leave as confident practitioners.
Final Thoughts on Your Professional Journey
Deciding to focus your energy on a specific modality is the most powerful step you can take. Whether you are drawn to the intensity of sports performance or the intricacies of clinical sports rehabilitation, the key is to seek out training that challenges you. Do not settle for a superficial education. By investing in fully qualified and accredited specialized education, you are securing a future where you can make a profound difference in the lives of your clients. At RSM International Academy in Chiang Mai, we are dedicated to helping you achieve that standard of excellence.
The Role of Massage in Rehabilitation and Recovery
At RSM International Academy, we approach bodywork through a strictly clinical lens. While the general public often views massage as a luxury, within sports medicine, it is a critical instrument for restoring function. While teaching RSM’s Remedial Massage Course in Chiang Mai, my objective is to bridge the gap between relaxation and therapeutic necessity. And an understanding of anatomy is key to transforming manual therapy into a potent catalyst for healing.
The Science Behind Massage Therapy and Rehabilitation
Physical trauma disrupts the body’s natural equilibrium. When injuries occur, inflammation protects the area but often leads to stiffness. Massage therapy acts as an external modulator of this process. It does not simply soothe; it mechanically alters the environment of injured tissues.
Massage therapy improves blood flow to the affected area. This circulation delivers oxygen vital for repair while flushing out metabolic waste. As a result, the biological timeline for tissue repair accelerates. Massage therapy can help reduce swelling by manually encouraging the movement of lymph fluid. Therapists use lymphatic drainage techniques to reduce fluid buildup, allowing patients to regain mobility sooner than they would with rest alone.
Accelerating Recovery and Managing Pain
Pain is the primary barrier to effective physical therapy. When a patient hurts, they guard the injury, causing compensatory patterns. Massage therapy is beneficial here because it creates a neurological distraction.
Manual manipulation stimulates mechanoreceptors in the muscles. This input can override pain signals sent to the brain. Consequently, the relief experienced allows for more aggressive physical rehabilitation. We also must address scar tissue. When tissue injuries heal, collagen fibers often form disorganized adhesions. Myofascial release helps realign these fibers. This leads to a functional scar that moves with the muscle. A massage intervention helped numerous patients in our practice avoid long-term stiffness by keeping tissue pliable during the remodeling phase.
Sports Massage in Modern Athletic Care
Athletes operate at the limits of human capability. For them, injury treatment is a race against time. Sports massage differs from standard therapeutic massage by targeting specific muscle groups to prevent repetitive strain.
In high-performance settings, massage therapy provides a competitive edge. It maintains optimal muscle length. Studies suggest that targeted soft tissue work can significantly increase vertical jump and power by reducing internal resistance. Sports medicine professionals rely on these techniques to manage micro-trauma. Recovery massage scheduled between sessions flushes out lactate. Conversely, ignoring this maintenance often leads to overuse injuries.
The Impact on Post-Surgical Patients
Surgery is a controlled trauma. The post-operative phase requires a nuanced approach. The rehabilitation process often involves immobility, causing atrophy. Benefits for surgical patients include:
- Improved Circulation: Speeds up wound healing by enhancing oxygen delivery.
- Adhesion Prevention: Prevents deep internal scarring that restricts movement.
- Pain Management: Triggers endorphin release to reduce reliance on painkillers.
Care during this stage must be coordinated with the surgeon. However, appropriate superficial work can stimulate flow without risking structural integrity.
A Holistic Approach to Injury Treatment
At our academy, a holistic approach means treating the entire kinematic chain. An injury in the knee often stems from hip instability. Treating only the knee is insufficient. Massage therapy allows the therapist to palpate tissue changes across the physical structure to identify the root cause. This leads to a treatment plan that fixes the dysfunction, not just the symptom.
The psychological aspect of recovery is equally significant. Physical trauma causes mental stress, keeping the body in a “fight or flight” state. Massage shifts the body into a parasympathetic state. This leads to an environment conducive to repair.
Whether for exercise recovery or post-operative care, the mechanical support provided by expert hands is irreplaceable. By managing pain, ensuring tissue alignment, and optimizing performance, massage remains a cornerstone of modern rehabilitation.
Myofascial Pain Syndrome Explained from a Sports Medicine Perspective
Pain is rarely a simple signal. In my years practicing sports medicine and training therapists at RSM International Academy, I have observed that the site of the pain is frequently not the source of the problem. Patients often arrive pointing to a throbbing shoulder or a burning lower back, convinced they have torn a ligament or damaged a disc. Often, the reality is less structural and more functional. They are dealing with a complex neuromuscular condition. Specifically, they are experiencing myofascial pain syndrome.
This condition is ubiquitous yet frequently misunderstood. It manifests as a deep, aching sensation that persists despite rest and standard interventions. Myofascial pain syndrome is defined by the presence of hypersensitive spots within the muscle, technically termed trigger points. In RSM’s Dynamic Myofascial Release Course, we teach that to understand this pathology, we must look beyond surface-level symptoms and examine the functional mechanics of skeletal muscle.
Defining Myofascial Pain Syndrome
Precision in diagnosis leads to precision in treatment. Myofascial pain syndrome (MPS) is a chronic pain disorder affecting the musculoskeletal system. It differs significantly from the temporary soreness one might feel after a heavy gym session. While delayed onset muscle soreness resolves within days, MPS persists. It is characterized by localized areas of deep tenderness and stiffness that can severely restrict range of motion.
The condition centers on the fascia and the muscle fibers themselves. When these tissues face repetitive stress or trauma, they develop specific hyperirritable spots located within a taut band of muscle. These spots are physiological contractures where muscle fibers have locked into a shortened state.
This contraction restricts local blood flow, creating a localized area of ischemia. Consequently, the tissue starves of oxygen and nutrients, leading to a metabolic crisis. This distress releases chemical substances that sensitize pain receptors, creating a self-perpetuating cycle of myofascial pain.
The Mechanism of Trigger Points
The engine driving this pain syndrome is the trigger point. At RSM International Academy, we teach that effective treatment relies on palpable identification. A trigger point is not a metaphorical “knot.” It is a physical reality. When you palpate the muscle belly, you feel a distinct, rope-like texture – the taut band.
Pressing on this nodule often elicits a “jump sign,” an involuntary reflex where the patient flinches due to the intense sensitivity. The formation of these points occurs at the microscopic level. The sliding filaments within the muscle fiber get stuck in a contracted position, often due to an excessive release of acetylcholine.
The result is a segment of muscle that works continuously, even during sleep. This constant contraction depletes adenosine triphosphate (ATP), the energy molecule required for muscle relaxation. Without ATP, the fibers cannot uncouple, and the metabolic waste accumulates. This chemical soup irritates the surrounding nerves, causing ongoing discomfort.
Understanding Referred Pain
A defining characteristic of MPS that confuses both the patient and the inexperienced doctor is referred pain. This phenomenon occurs when pain is perceived in a part of the body separate from its actual source. The brain misinterprets nociceptive signals, projecting the sensation along shared neural pathways.
For instance, a trigger point in the upper trapezius frequently sends pain signals into the temple, mimicking a tension headache. Similarly, trigger points in the glutes can radiate down the leg, masquerading as sciatica. If a therapist treats only the area where the patient feels pain, the treatment will fail. We must trace the symptoms back to the primary generator.
Recognizing these patterns is a fundamental skill.
- Sternocleidomastoid: Refers to the eye and ear.
- Infraspinatus: Refers deep into the shoulder joint.
- Quadratus Lumborum: Refers to the hip.
Diagnosis and Clinical Assessment
Diagnosing MPS requires a hands-on approach. Standard imaging studies like MRIs or X-rays do not reveal trigger points, often leading to frustration for patients who are told their scans are normal despite their agony.
A skilled clinician relies on palpation to identify the following:
- A tender spot within a taut band.
- Reproduction of the patient’s familiar pain.
- A local twitch response when the band is snapped.
This assessment distinguishes MPS from fibromyalgia. Fibromyalgia is a systemic condition with widespread sensitivity, whereas myofascial pain is regional and originates from specific, palpable nodules.
Treatments for Myofascial Pain
At our center, we advocate for a multimodal approach. Effective treatment requires a combination of manual therapy, mechanical intervention, and movement correction.
Manual Therapy: Techniques like ischemic compression are the cornerstone of care. By applying sustained pressure to the trigger point, we temporarily halt blood flow. Upon release, fresh, oxygenated blood rushes into the tissue, flushing out inflammatory metabolites. Myofascial release further aids in unsticking the connective tissue layers, restoring the slide-and-glide potential of the fascia.
Dry Needling: For deep or stubborn points, dry needling is a powerful modality. This involves inserting a thin needle directly into the trigger point to elicit a twitch response. This reflex rapidly depolarizes the muscle fiber, effectively hitting the “reset button” on the dysfunctional tissue. While the sensation can be intense, the relief from chronic myofascial tightness is often immediate.
Chronic Pain and Sensitization
If left untreated, this condition can become a long-term pain condition. The constant bombardment of pain signals sensitizes the central nervous system. The threshold for feeling pain lowers, meaning stimuli that should be harmless become painful.
This is why we emphasize early intervention. We must interrupt the cycle before it alters neural architecture. A longer-lasting muscle pain requires a comprehensive strategy that addresses not just the tissue, but the nervous system’s interpretation of danger.
The Role of Posture and Biomechanics
Treating the symptom without addressing the cause is futile. Poor ergonomics and repetitive strain are leading contributors to myofascial trigger points. Sitting with a forward head posture places immense strain on the neck muscles, forcing them into a state of semi-contraction.
We analyze the patient’s movement patterns. If the shoulders are rounded or the pelvis is tilted, we must correct these structural deviations. We prescribe corrective exercises to lengthen shortened muscles and strengthen weak ones. This restores balance to the kinetic chain. For example, treating back pain often requires releasing tight chest muscles that are pulling the posture forward.
Patient Education and Self-Care
Information is a vital component of recovery. When a patient understands that their pain stems from a solvable mechanical issue rather than permanent damage, anxiety decreases. We empower patients with self-care tools.
Self-Myofascial Release: Using foam rollers or lacrosse balls allows patients to apply pressure to trigger points at home.
Stretching: Gentle elongation prevents the taut band from reforming.
Heat: Applying heat improves blood flow and relaxes the muscle before stretching.
Consistency is key. A single appointment at a clinic provides relief, but daily maintenance ensures long-term resolution.
Final Thoughts on Management
Myofascial pain syndrome is not a life sentence; it is a functional puzzle. With the right combination of hands-on skill, anatomical knowledge, and patient cooperation, it is highly treatable.
For therapists, mastering the diagnosis and treatment of myofascial pain transforms you from a technician into a true clinician. For patients, understanding the mechanism of your pain is the first step toward reclaiming your movement. At RSM International Academy, we believe that identifying the source, rather than chasing the symptom, is the essence of elite sports medicine.
Exploring Career Paths After Sports Massage Certification
The perception of manual therapy has shifted drastically. At RSM International Academy in Chiang Mai, we witness this evolution daily. Students arrive not merely to learn a routine, but to master the mechanics of the human body. The industry no longer limits practitioners to luxury spas. Instead, a rigorous education in sports massage opens doors to high-level performance and clinical rehabilitation.
We founded this school on evidence-based practice. My background in sports medicine dictates the curriculum of RSM’s Sports Massage Course and, consequently, where our graduates go. When you master physiological responses to manipulation, you possess a skill set in high demand across the healthcare spectrum.
The Evolving Role of Massage Therapists
The modern practitioner is a clinician first. While stress reduction is valid, the current market demands functional improvement. Massage therapists are expected to solve problems, such as range-of-motion limitations or chronic pain patterns.
Addressing these issues requires deep pathophysiology knowledge. We teach students to assess tissue quality and apply targeted force to elicit healing. This technical proficiency separates a generalist from a specialist. A specialist does not just rub muscles; they manipulate the neuromuscular system.
This shift changes your professional trajectory. You provide a necessary health service. As a result, the venues where you can apply your trade expand. If you can reduce recovery time for an athlete or alleviate back pain for an office worker, you will find ample work.
Opportunities in Hospitals and Clinical Settings
One of the most rapidly growing sectors is the medical field. Hospitals and medical centers increasingly hire manual therapists to work alongside orthopedic surgeons and pain management specialists. Doctors recognize the value of soft tissue mobilization in post-operative recovery.
In a hospital setting, the work is precise. You might treat a patient recovering from a knee replacement, managing edema without disrupting the surgical site. This requires advanced knowledge of lymphatic drainage and contraindications. The reward is significant: you operate as a vital part of a care team, directly contributing to patient outcomes.
Integration with Physical Therapy
Closely related to hospital work is the collaboration within physical therapy clinics. Physiotherapists often focus on exercise prescription and joint mobilization but lack the time for extensive soft tissue work. This creates a perfect symbiosis.
In this model, the massage therapist handles soft tissue preparation. You release hypertonic muscles that prevent patients from performing corrective exercises. Once the tissue is pliable, the physical therapist takes over. This collaborative approach often yields faster results. Working here exposes you to conditions like rotator cuff tendinopathy and plantar fasciitis, acting as a form of daily continuing education.
The Reality of Sports Massage in Athletics
For many, the dream is working with elite athletes. While this is the core of RSM’s curriculum, the reality of sports differs from the glamour portrayed in media. It is fast-paced and demands exceptional problem-solving.
When working with a team, you are part of a performance unit. The coach needs the player on the field; the trainer needs the athlete to hit metrics. Your job is ensuring the soft tissue health to make that happen.
Pre-event massage must stimulate the nervous system without reducing muscle tone. Post-event work focuses on flushing metabolic waste. Between events, you handle maintenance, breaking down adhesions from repetitive strain. High-level fitness facilities demand therapists who understand biomechanics. If treating a runner, you must understand the impact forces on the posterior chain. We train you to think like a mechanic for the human engine.
Building Success in Private Therapy Clinics
Entrepreneurship represents a significant avenue. Opening your own clinic allows you to define your philosophy. However, running therapy clinics requires business acumen and a clear market position.
In a private setting, you have the freedom to specialize. Specialization builds reputation. Whether focusing on runners or neck pathology, becoming the “go-to” person creates a stable client base.
At RSM, we view practice as a healthcare service. Your intake process should be thorough, and your documentation clinical. Clients return because you explained the source of their pain and resolved it, not just because the environment was relaxing. Successful private practitioners often build referral networks with chiropractors and osteopaths, establishing trust through consistent clinical results.
Defining Your Career Options
The versatility of a sports massage certification means you are not locked into a single trajectory. Career options abound for those dedicated to their craft.
Some graduates combine manual skills with other disciplines, becoming personal trainers or yoga instructors. This hybrid model attracts clients wanting a single point of contact for health and fitness. Others move into education, teaching the next generation. Schools always seek experienced instructors who can articulate complex concepts.
Corporate wellness is another emerging field. Companies hire therapists to provide on-site treatments and ergonomic assessments to reduce costs associated with repetitive strain injuries. This role combines manual therapy with employee education.
How the Work Defines the Professional
Regardless of the setting, this work is physically and mentally demanding. It is a labor of intention. You must listen to the tissue with your hands.
A successful massage therapist protects their greatest asset: their body. Biomechanics are crucial. If you cannot generate force using your core, your career will be short. At RSM, we drill body mechanics relentlessly. Learning to work from your center allows you to treat multiple clients without burnout.
The Importance of Education
The barrier to entry in this industry varies, but the barrier to success is uniform: quality education. A weekend workshop does not prepare you to rehabilitate a torn hamstring.
We emphasize a deep dive into anatomy and kinesiology. You need to know where nerves run to avoid compression. This knowledge gives you confidence. When a client asks about their pain, you provide a physiological explanation. Continuing education is mandatory; to stay relevant, you must stay informed about the latest research in fascia and pain science.
Evaluating the Market
The demand for massage services grows as the population ages and remains active. “Weekend warriors” – amateur athletes in triathlons or CrossFit – treat their bodies like machines. They view massage not as a luxury, but as maintenance.
This shift in consumer behavior drives employment prospects. Furthermore, the medical community’s search for non-pharmacological pain management places massage therapy in a strong position. Insurance providers are increasingly recognizing this value.
Summary of Potential Environments
- Clinical Settings: Aiding post-operative recovery alongside surgeons.
- Rehabilitation: Partnering with physical therapists for functional restoration.
- Professional Athletics: Serving on performance teams to prevent injury.
- Private Practice: specialized business focusing on specific pathologies.
- Corporate Wellness: On-site care to improve employee health.
- Education: Teaching through accredited massage school programs.
The landscape of massage therapy is vast, and the path you choose should align with your temperament and your passion. However, all these paths require the same fuel: excellence in practice and a dedication to the science of the human body.
Common Shiatsu Massage Misconceptions: An Evidence-Based Perspective
Patients often arrive at our clinic with rigid expectations. They anticipate either a gentle, oil-based spa experience or a punishing session of “deep tissue” work. These expectations stem from a fundamental lack of understanding regarding the physiological aims of clinical manual therapy. In RSM’s Deep Shiatsu Massage Course, we address these inaccuracies. We teach that sports medicine requires precision, not just intensity or relaxation.
To appreciate the true clinical value of this modality, we must dismantle the prevailing myths. Treating Shiatsu as purely recreational undermines its potential to treat orthopedic conditions. I aim to clarify these points using my experience in sports medicine and the anatomical realities of the human frame.
Defining Shiatsu Therapy Within Sports Medicine
Shiatsu is often misclassified alongside general wellness treatments. The term literally translates to “finger pressure,” but the technique is far more sophisticated. It involves using thumbs, palms, and elbows to apply perpendicular pressure to specific points. While traditional texts reference energy channels, modern sports medicine interprets these as neuroanatomical points and trigger points.
Shiatsu therapy is a calculated manipulation of soft tissue. In our curriculum, we emphasize that the practitioner engages with the fascia and the nervous system. Shiatsu is not a passive routine; it is a diagnostic tool. A skilled practitioner reads tissue texture and tension to assess the athlete’s condition. Shiatsu needs to be viewed as a communicative loop between the therapist and the patient’s nervous system. When we strip away esoteric language, we find a potent tool for rehabilitation.
Myth: Effective Treatment Must Be Painful
The “no pain, no gain” mentality plagues the recovery world. Many believe that if a treatment doesn’t hurt, it isn’t working. This is a dangerous fallacy. There is a vast difference between “good pain”—a sensation of release—and the “bad pain” that triggers a defensive response.
Shiatsu is generally not painful when performed correctly. Inflicting sharp pain activates the sympathetic nervous system. As a result, muscles contract to protect the area. If a therapist fights this guarding response, they risk damaging the tissue.
Pressure must be modulated to bypass this defense. Shiatsu practitioners sink their weight gradually, allowing the parasympathetic nervous system to engage. This signals the muscles to relax, allowing for deeper access without trauma. Deep tissue massage is often requested with the assumption of aggressive force, but true depth requires patience. If a patient winces, the treatment is failing.
Myth: Massages Are All the Same
The public often groups all manual therapies together, ignoring mechanical differences. Swedish massage relies on gliding strokes using oil to affect fluid dynamics. Massages are all distinct in their mechanics. Shiatsu styles differ fundamentally because they are typically performed without oil on a fully clothed client.
This absence of lubrication is clinically significant. Without the glide of oil, the therapist can anchor the tissue. This allows for specific shearing forces that are impossible on slippery skin. Shiatsu effects are structural. By fixing a point and applying static pressure, we can mechanically lengthen short fibers.
The Physical Benefits for the Body
Another limiting belief is that manual therapy is for relaxation only. While stress reduction is valuable, clinical massage offers much more. We must shift our perspective to functional restoration.
Massage can help balance the autonomic nervous system, but the effects on the muscles are equally profound. Benefits of consistent Shiatsu include improved joint mobility and the breakdown of scar tissue. Massage therapy acts as a vital component of medical recovery plans. At RSM, we view the body as a kinetic chain. Shiatsu allows us to trace lines of tension to treat the root cause of pain.
Wellness is about maintaining a functional physiological state. Conditions like tension headaches often have somatic origins. By regulating muscle tension, Shiatsu addresses these dysfunctions. It is a form of complementary medicine that works alongside orthopedic care.
Choosing the Right Massage Therapist
Treatment effectiveness depends entirely on the provider’s skill. Shiatsu needs to be administered by someone who understands anatomy. Massage therapists are not interchangeable. A practitioner with superficial training lacks the diagnostic acumen of a sports medicine specialist.
At our clinic, we emphasize that hands-on skill must be backed by theory. If a therapist cannot explain the anatomy they are treating, the effectiveness is compromised. Therapists must also possess the physical conditioning to deliver consistent pressure.
Patients should verify the credentials of their practitioners. Alternative medicine is a broad field, so finding a specialist who understands Western anatomy is essential. Massage myths persist because patients receive substandard care. By understanding what Shiatsu truly is, patients can make informed decisions for their recovery.